Earlier this week, on a New York subway train, a woman did something that caused me to descend into nothing short of sheer panic: She dropped a melon. It rolled down the car thunderously, careening past the ankles of passengers, until it landed right in front of my feet. My first instinct was to be a good citizen and to pick it up and deliver it to its owner. But a small, nagging voice in the back of my mind that’s grown louder and louder as of late advised me not to. So, instead of actually handing it over to her, I gingerly kicked it over to her. To her credit, she didn’t seem fazed: She picked it up and gave me a thumbs-up.
I spent hours obsessing over this interaction. That’s in part because, a few minutes after this interaction, I thought I spotted the woman who’d dropped the melon surreptitiously coughing, and in a news cycle drenched in constant updates about COVID-19, I was delirious with panic: Had I touched my foot that had touched the melon? Was I outside of the range of six feet required for coronavirus transmission, per the CDC, of the woman who had dropped it? Did I brush past her when I got off the train? Had I washed my hands thoroughly enough when I got off the subway? Had I Purell’ed them thoroughly enough? Would I run out of Purell soon and be unable to afford it now that resellers on Amazon had jacked up the price?
But mostly I just felt guilty about it. I’m not the most socially adept person on the planet, but I still am not in the habit of kicking other people’s personal items when they’re in my line of vision. Had COVID-19 and the ensuing panic fucked with my mind to the degree that basic social morés were just flying out the window?
Truthfully, prior to the advent of COVID-19, I probably would’ve gone through this thought process. I have diagnosed obsessive-compulsive disorder (OCD), an anxiety disorder that manifests itself in obsessive, unwanted thoughts and compulsive behaviors; for me, as is the case for many people with OCD, mine manifests itself in obsessive fears of myself or my family members getting sick, with a healthy dose of germophobia thrown in for good measure.
When the CDC announced its list of best practices for preventing COVID-19, my first thought was that years of engaging in obsessive behaviors such as ruminating on protective measures or washing my hands till they cracked and bled would better equip me for the impending apocalypse. But as the weeks have passed and the virus has spread, with deniers on one side of the spectrum and alarmists on the other, it’s been difficult to ignore just how much the symptoms of my OCD have been exacerbated by the intense media coverage. This is likely true for many people who struggle with anxiety disorders, an umbrella term that describes everything from generalized anxiety disorder to panic disorder to obsessive-compulsive disorder (OCD).
“It’s coming up a lot. In fact, I had a session on it this morning,” says Dr. Nicole Naggar, a psychiatrist in New York. “For those of us who may be more slanted in an anxious way, we can be really vulnerable to the news, especially if we happen to be germophobes too.” Angelina, an immunocompromised person struggling with OCD, whose last name has been withheld at her request, concurs. Angelina lives in Washington state, where an estimated nine people have died from a COVID-19 outbreak, which has exacerbated her fears. “I’ve been trying to stay optimistic but it’s so hard to do when the media is creating this hysteria,” she says.
People with anxiety disorders comprise a sizable percentage of the population. According to the Anxiety and Depression Association of America, nearly 18 percent of the population, or 40 million adults, struggle with some form of anxiety disorder.
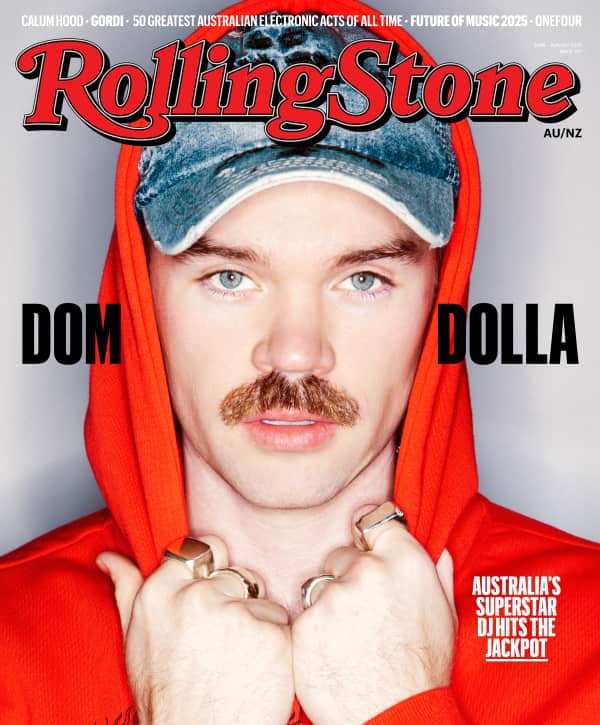
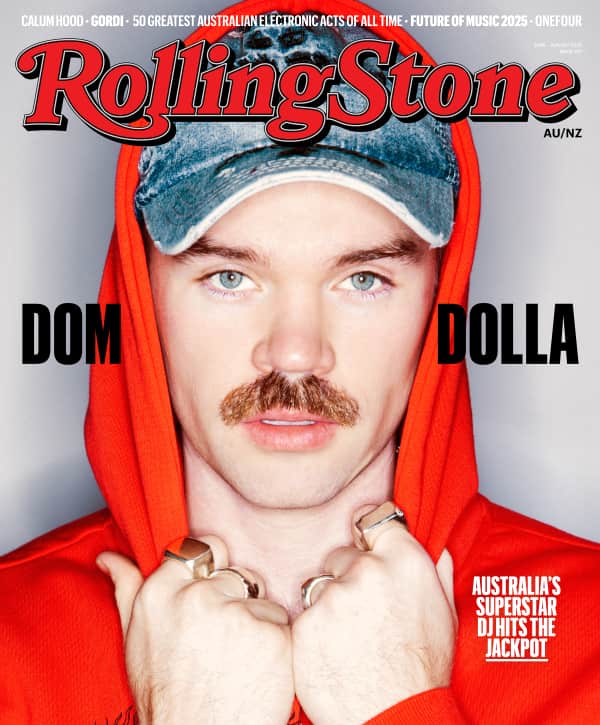
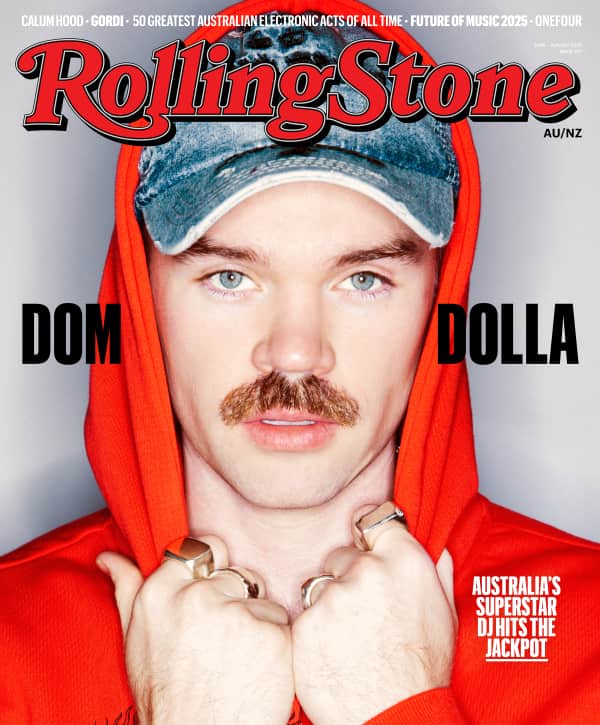
Love Music?
Get your daily dose of everything happening in Australian/New Zealand music and globally.
Of course, even for those who don’t have a formal diagnosis, the wall-to-wall news coverage of the virus now known as COVID-19 is immensely concerning — and there’s some data to indicate that pandemics can wreak havoc on the general population’s mental health. In the past, depression and anxiety rates have soared following terrorist attacks, even among those who were not directly impacted.
Yet for those predisposed to anxiety, it could prove immensely triggering, says Dr. Robert Schachter, assistant clinical professor at the Icahn School of Medicine at Mount Sinai. “Think of anxiety as this underground river that’s flowing all the time,” he says. “If you have a ‘What if?’ thought” — a fear-inducing hypothetical scenario prompted by headlines about price-jacking on hand sanitizer or photos of abandoned grocery stores in Milan — “then that pokes a hole and gives a reason for the anxiety to come out.”

A trader passes a hand-sanitizing station on the floor of the New York Stock Exchange. Photo credit: Richard Drew/AP/Shutterstock
Because there’s relatively little known about COVID-19, there’s a great deal of uncertainty surrounding the virus — and uncertainty, if nothing else, breeds “What ifs.” Even those who don’t necessarily have an anxiety disorder may find themselves felled by such thoughts, says Naggar, who says it is “absolutely possible” that news of coronavirus “could be an exposure or a trauma of sorts that could trigger” them.
Since news of COVID-19 first broke in the United States in December, media coverage has essentially been wall-to-wall. The vast majority of such coverage has centered on what we know about the virus, as well as the administration’s questionable handling of the ensuing health crisis, with President Trump most recently telling pharmaceutical executives to come up with a cure and vaccine all in one. (The World Health Organization (WHO) has said that it will take at least 18 months to develop a vaccine to COVID-19.) Yet very little has focused on the mental health effects of the omnipresent threat of coronavirus, which, combined with the administration’s response to COVID-19, creates “a perfect cocktail” of fear, says Dr. Chloe Carmichael, a clinical psychologist in New York. With previous health crises like SARS and the Ebola virus, the response was not highly politicized. Now, with COVID-19 being touted by right-wing media figures as a call to close borders, “it does seem like the administration’s handling of it has become a political football, which almost kinda supercharges the anxiety about it, says Carmichael.
That’s to say nothing of how little coverage has been afforded to the day-to-day experiences of those in countries where the crisis is more acute, such as China, Japan, Iran, and Italy, where the psychological impact of living with the threat — not to mention the isolation of quarantine — is immense. And there is evidence to suggest that the fallout could linger long after panic over the virus (hopefully! fingers crossed!) recedes. Studies of survivors, health care professionals, and members of surrounding communities impacted by the SARS crisis in Asia and Canada found that people were struggling with mental health issues up to four years after the epidemic had passed. Other studies post-9/11 found that watching news coverage of the attacks produced “substantial stress symptoms,” even in those who were watching from hundreds of miles away.
For those who struggle with anxiety disorders, part of the difficulty of dealing with coverage of COVID-19 stems from being unable to discern between the genuine threat posed by the illness and the inflated threat perpetuated by hysterical media coverage. Schachter refers to these two types of anxiety as “Anxiety One” and “Anxiety Two.” “With the virus there’s a lot of Anxiety One because it is dangerous in some cases,” particularly for the elderly or immunocompromised, says Schachter. “But we really don’t know the extent of it.” Such uncertainty creates prime conditions for the development of Anxiety Two, allowing people to “jump into the void” and make negative assumptions that are unrelated to the actual probability of contracting or dying from the virus, says Schachter. And this is likely especially true for marginalized people such as low-income people or people of color, who are often more likely than members of the general population to have anxiety disorders and less likely to have access to treatment like cognitive behavioral therapy or medication.
To complicate matters, many people with anxiety disorders adopt compulsive behaviors as a way to alleviate their own obsessive concerns, such as hand-washing or rigorously applying Purell an inordinate number of times a day to avoid contracting illness. Because these are the exact same behaviors recommended by the CDC to avoid contracting COVID-19, that can be confusing and disorienting for people with anxiety to discern between rationally and irrationally motivated behaviors. There’s a distinction between adhering to CDC guidelines as a way to keep yourself safe and doing so in a problematic way, says Carmichael. “If you keep excusing yourself to wash your hands on a date and it starts to interfere with your ability to focus on things, that’s a sign it’s starting to get a little bit overboard,” she says. It’s also a sign you may want to talk to a mental health care professional.
For those who are already finding themselves crippled by anxiety related to coronavirus, however, the question is: How can they alleviate some of that concern, without burying their head in the sand regarding the actual risk? The answer, says Schacter, is not to avoid media coverage of the virus (not that that would really be possible for those of us with access to WiFi, anyway). “Avoiding the media doesn’t help,” he says. “If you get anxious looking at the media, say, ‘Time out, I’m uncomfortable and anxious, let’s look at how realistic my fears are,’ and go through the steps of assessing that.”
That said, it’s probably more helpful to rely on trustworthy outlets (think the actual CDC and WHO websites, not something your uncle posts on Facebook) and steer clear of the types of headlines that are engineered specifically for the purposes of generating clicks, not to help you assess your actual risk level. For me, identifying such content is like identifying pornography: I know it when I see it. “The best coverage I’ve seen is from scientists that actually explain the virus and what it does in our bodies so we can identify it quickly — thus resulting in preventing its spread through proper education and awareness,” says Angelina. “Not stories scaring the shit out of everyone and urging them to clear out their grocery stores.”
Above all else, now is the time to rely on facts and hard data, both of which are far more reassuring than most media coverage would otherwise suggest. “The fantasy versus the reality of COVID-19 are very different,” says Naggar. For me, it’s been helpful to memorize these statistics the way old white men do 1950s baseball team starting lineups: Thus far, the fatality rate of the virus is two percent, higher than that of the flu but lower than that of, say, SARS (10 percent) or MERS (30 percent). More than 80 percent of coronavirus cases are mild, which has made it easier to spread, but also may potentially render the carrier immune to developing it again in the future. Only 1.2 percent of the overall number of cases in China were among people between the ages of 10 and 19, indicating children are largely protected (a huge relief to parents such as myself); and the elderly and infirm are far more at risk of developing more serious cases, though falling into just one of those categories is not a death sentence in and of itself. (“A healthy 72-year-old is not at as great a risk as an unhealthy 72-year-old,” the health officer for Sacramento County told the Los Angeles Times.)
In short, there is real risk, but for the vast majority of us, the risk is not commensurate with the degree of obsession and panic coverage of the virus has bred, both in people who are panic-prone and those who are not. Is this to say I’ll start licking melons the next time one rolls across a subway car floor? Probably not, but it is a case for looking someone in the eye and handing it back to them like an actual human being — even if you do apply Purell right after.
If you are struggling with mental health conditions, please reach out to a mental health care professional or contact the National Association of Mental Illness (NAMI) Monday through Friday from 10 a.m. to 6 p.m. EST at 800-950-NAMI (6264).