Thanks to advancements in medicine, skin care, and elective cosmetic treatments, our picture of aging has changed radically over the past several decades. More people are dyeing their hair when it turns gray, and we now have a better understanding of the impact of exercise and nutrition on both physical appearance and longevity than ever before. Between 1959 and 2014, life expectancy in the U.S. rose from 69.9 years to 78.9 years (though it has since plateaued and decreased slightly). In other words, being 70 in 2020 looks and feels a lot different than being the same age even just one generation ago.
And then came COVID-19. All of a sudden, people aged 65 and older were collectively labeled as “high risk” — regardless of their actual health status — and instructed to stay home and take extra precautions. According to Dr. Karen Fingerman, professor of human development and family sciences at the University of Texas, Austin, this categorization stems from the impact COVID-19 has had on residents of nursing homes. “There’s no doubt that the death rate in nursing homes is astronomical, but when you look at the statistics, only five percent of older adults are in nursing homes,” Fingerman tells Rolling Stone. “They’re very high risk, but [the residents are] incredibly sick and frail to begin with. So we’re talking about high susceptibility, but we’re talking about a fairly small portion of the older adult population.”
A recent article in the Journal of the American Medical Association on COVID-19 deaths in Italy helps to illustrate this point. According to the study’s findings, the rate of death for 60- to 69-year-olds was three to four percent — only slightly higher than the general population — but jumped to 20 percent for those over the age of 80. “We have an extremely vulnerable population that has suffered the brunt of the deaths in the nursing homes,” Fingerman explains. “But generalizing that to say it’s all older adults presents a view of old age that is very deteriorated.”
Instead, Fingerman suggests that we start thinking more like age researchers, who consider both biological and chronological age. As she recently explained in an op-ed in USA Today, “Chronological age is the number of years since birth.… Biological age reflects the physiology of a person and how well that person is functioning.” In the case of COVID-19, biological age matters most when it comes to the risk of serious illness or death. Putting all adults chronologically age 65 and older in the same category stigmatizes the entire group, regardless of individual health status.
“Of course, you cannot evaluate each and every individual these days, given the crisis situation,” says Dr. Daniela Jopp, an associate professor of psychology at the Université de Lausanne in Switzerland who specializes in aging. “But I think it’s very important to keep in mind that, yes, we want to protect people whose risk is higher due to their age, but that it should not have a larger impact in the sense that older people could be treated like second-class citizens [in the future].”
In the midst of a global pandemic, everyone is in some version of survival mode. And as it turns out, grouping all older adults together and labeling them as high risk is, for many, a coping mechanism. “When something like a pandemic happens, not only do we look for someone to blame, we also look for a way to protect ourselves from the possibility that this could happen to us,” says Dr. Gilad Hirschberger, associate professor of psychology at the Interdisciplinary Center in Israel. Since the pandemic mainly affects older people, it provides those under 65 with a form of “psychological protection,” he says. “We can say, ‘It’s not us.’”
But older adults aren’t a homogenous group. “There’s so much more diversity in the older adult population in comparison to younger populations, and that includes older adults being diverse in a variety of ways across race, ethnicity, socioeconomic status, disability, sexual orientation, and gender identity,” Dr. Katherine Ramos, an assistant professor in psychiatry and behavioral sciences at Duke University who specializes in aging tells Rolling Stone. We know, for example, that communities of color are disproportionately impacted by COVID-19. When members of these communities get older, they not only have to deal with the stigma of aging, but also the existing health disparities that come with being part of their racial or ethnic group. In other words, health care may be more accessible to a white, middle-class 70-year-old than someone of the same age who is of another race, ethnicity, or socioeconomic status. “We need to focus on the nuance of the diversity of older adults, and how within that diversity, some [people] will have more privileges than others,” Ramos says.
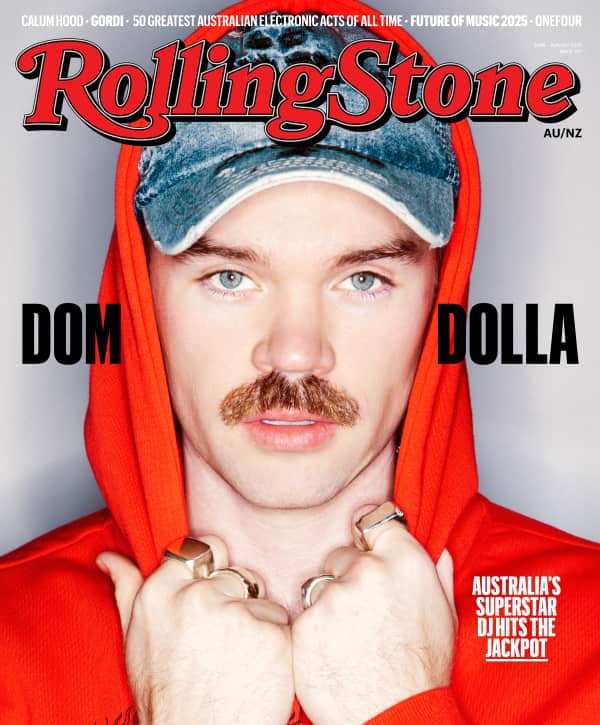
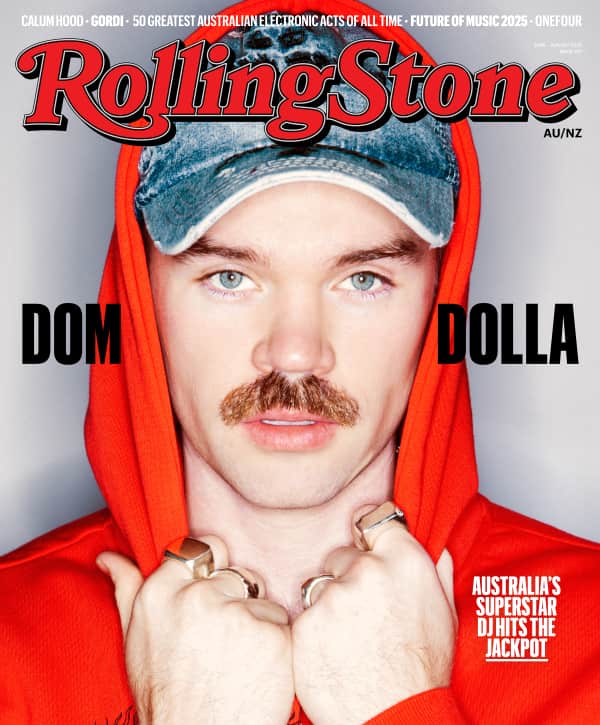
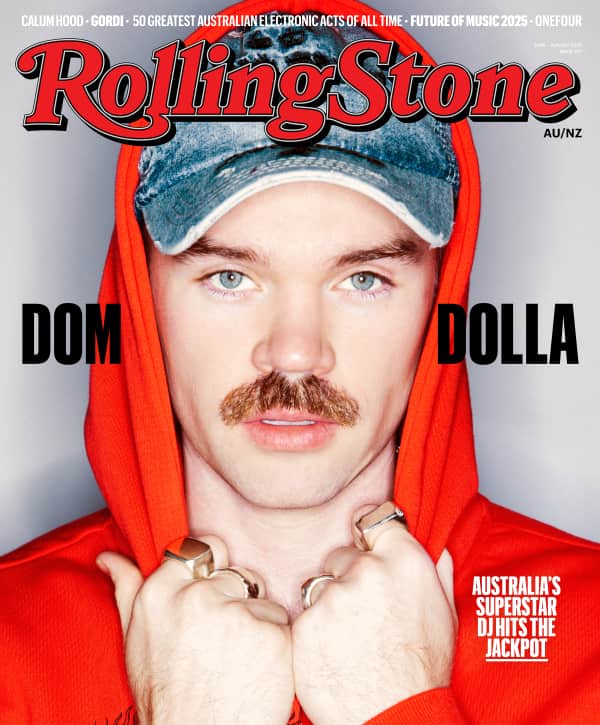
Love Music?
Get your daily dose of everything happening in Australian/New Zealand music and globally.
And when weighing options like the risks and benefits of reopening public life, or who should get a ventilator when supplies are limited, we are assigning varying degrees of value to the lives of other human beings — whether or not we realize it. Yes, reopening society may boost the economy, but doing so too soon may bring on a second wave of the virus, adding to the already-high COVID-19 death toll among adults over the age of 80. Earlier in the pandemic, when states and hospitals discussed the allocation of ventilators in the case of a shortage, some of the proposed guidelines prioritized younger people. Even though most health care facilities didn’t get to the point of having to make these decisions, the implication of the conversation — that older adults may be less deserving of lifesaving health care — lingers. “It’s kind of like a massive experiment in the psychology of morality: You have to choose between saving the economy and saving older people. It really places people in this moral dilemma,” Hirschberger says. “Older people are double victims. On the one hand, they’re victims of the real disease. They’re also victims of societal attitudes that say ‘You’re expendable.’”
And it doesn’t help that many don’t consider later years as valuable as younger years. “If you lose a decade from 30 to 40, that seems more significant than losing a decade from 80 to 90,” Hirschberger says. “But who’s to say — it’s still a life, and it’s still valuable.” According to Ramos, many of the current discussions surrounding the virus and health care rationing are devaluing older adults’ lives. “We need to take a moment to pause and think about how this pandemic might be inadvertently perpetuating stereotypic beliefs that being an older adult means that you don’t have something to contribute to society,” she says.
But by “othering” older adults, we’re actually harming ourselves. “Coronavirus and aging have something in common: No one is immune from either. The fact is, COVID-19 is having devastating impacts on people no matter age, geography, or any other characteristic,” AARP CEO Jo Ann Jenkins tells Rolling Stone. “Ageism is a strange phenomenon — it’s prejudice against your future self. The answer on all counts is to take good care of yourself and others. We are all in this together.”
As humans, we really don’t like to think about our own mortality, and the COVID-19 pandemic is making us do just that — regardless of our age. “Part of our denial of death is ageism, because if we were to accept death, we would look at old people and say, ‘That’s me tomorrow,’” Hirschberger says. “But if we deny our connection to that, then we have these negative attitudes toward people who are most vulnerable. There’s a paradox: On the one hand, everybody wants to live a long and healthy life. Yet, when we’re in a situation like this, we’re very quick to give up on other people’s chance to live a long life.”
So where will this leave us post-COVID-19? Once you actively stigmatize an entire demographic and assign them less value than other human beings, it sets a dangerous precedent that isn’t easily reversed. “I’m afraid that some of this ageism is going to stick around,” Hirschberger says. “This existential threat that has been elevated is going to make us want to draw the line, much more clearly and say, ‘Those are the people who aren’t like me, they’re older, they’re different, and they’re expendable.’”
On top of that, once the pandemic is over, the transition to some version of normal likely won’t be as straightforward for older adults. As Dr. Boaz M. Ben-David, associate professor of psychology at the Interdisciplinary Center in Israel and the University of Toronto, points out, once employers start the rehiring process, they are less likely to hire people in their 60s and 70s. In other words, even after the COVID-19 outbreak ends, its residual effects on older adults will continue: They will have access to fewer jobs, and in turn, less financial security. And it’s more than that: “Even if people don’t necessarily need a job in order to make money, they still need to work for the cognitive challenge, social interaction, and to have meaning in life,” Ben-David tells Rolling Stone.
But, as Jopp points out, the pandemic could also have a lasting positive impact on our view of aging, because it has provided increased opportunities for people to spend time with older people in their family and community. In fact, in Jopp’s previous research, she and her colleagues found that when people have a role model of successful aging in their life and have close contact with that person, it can give them a more positive perception of their own aging process.
Similarly, Fingerman is currently working with undergraduate students on a project which pairs older and younger adults. “But it’s not based on the idea that older adults are needy,” she says. “It’s based on the idea that older adults have wisdom and experience, and something to offer the conversation. I do think it’s important to help the older adults who are frail and living alone — if they need help — and there are volunteers doing that, and that’s important. But I think the other side of that is that there may be opportunities for connection.”
And beyond simply making a connection with another person, we have so much to learn from this segment of the population. “Older individuals have fought fights and won them. Instead of turning our backs on older adults, let’s turn our faces towards them and ask them about their resilience — how they were able to get over previous disasters in their lives,” Ben-David says. “These are the people that know how to bounce back. Let’s hear their stories about resilience instead of giving up on them.”