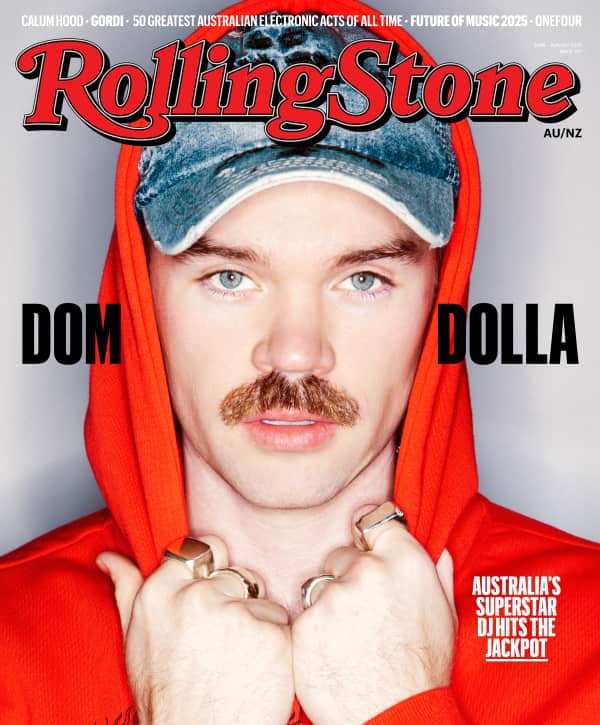
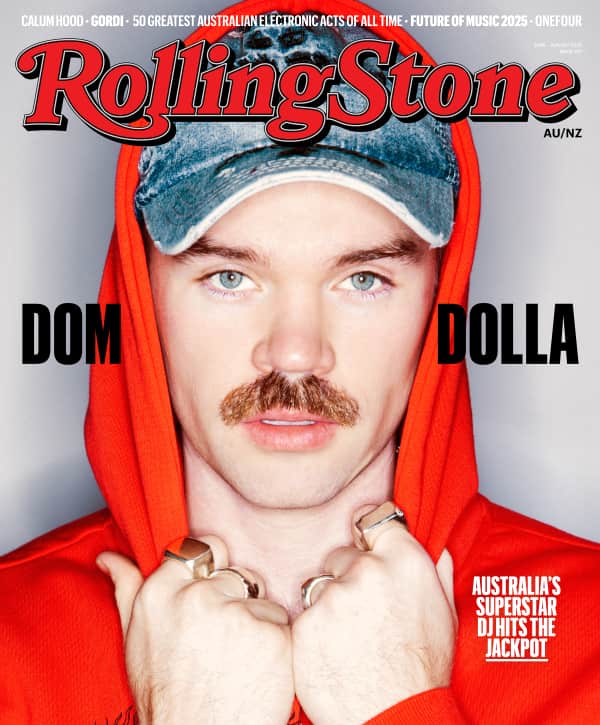
Kean Leanfore for Rolling Stone
Trans culture may be experiencing a tipping point, but it’s no thanks to Australia's current legislation.
Trigger warning: this content may be disturbing to some people as it contains references to self-harm.
Shanaya was seven years old when she started to question her upbringing and surroundings. Born to a traditional joint Indian family in Ahmedabad, her three cousins were more like her sisters, and men in the household were laughed at if they used the kitchen or prepared their own food.
“I started asking questions like, ‘Why am I not wearing clothes like my sister?’, ‘Why am I not able to do my hair like my sisters?’,” she recalls, when I visit her in Sydney. “But at the same time, I was afraid to ask because India back then was very reserved.”
At 32, Shanaya has experienced enough heartache and tragedy to make best-selling memoirs blush. When Shanaya moved to Melbourne with her partner Shweta 12 years ago, she was relieved. She felt Australia’s anti-discrimination laws would protect her and that the country’s progressive lawmakers and medical sector would ensure she lived happily and healthily as a transgender female.
For a while at least, this felt true. Shanaya and her partner lived in bliss and acceptance. Shweta would buy her feminine clothing, do her makeup, and encourage her to cook and clean – tasks which felt indulgent given her upbringing. They made plans for Shanaya to freeze her sperm so they could have children after her surgery. Shanaya’s affirmation surgery, or “bottom surgery” as it’s often called, will see the surgeon perform a vaginoplasty, taking her current genitalia and altering it to create both an outer and inner vagina.
In 2012, those plans were dissolved in a moment of sheer destruction. Shweta died in a car accident on a Californian highway when a semi-trailer truck T-boned the car she was in with her friends.
Ten days after Shweta’s death, Shanaya was on an escalator in a mall in Melbourne. She had been experiencing painful migraines from the grief and hadn’t been sleeping. She blacked out as one particular migraine seared through her skull. She fell shoulder first, fracturing bones in her legs and shoulders, resulting in a herniated disk. She woke up in a hospital where she could only move her left thumb.
Her sense of self was lost.
Love Music?
Get your daily dose of everything happening in Australian/New Zealand music and globally.
“I realised the only person who knew who I was, who accepted me how I am, was gone,” she remembers. “I didn’t have the courage to tell anyone what I was going through. Not only had I lost the love of my life, but I also lost the chance of becoming the person I wanted to be.
“I lost my purpose of living. I tried to harm myself. I went to Coles. I bought a knife and I went to the park. I waited for the dark.”
It was 3:30am when a stranger spotted Shanaya in the park with a knife. They made a call to police that saved her life. Shanaya spent almost a month in a psychiatric ward and was treated for gender dysphoria. But with no one in her personal life looking out for her, her application for permanent residency in Australia had gone unchecked. When Shanaya was released from hospital she found a letter noting she was currently residing unlawfully in Australia. She called immigration and was taken to Villawood Immigration Detention Centre. She was given the option to take the next flight out to India.
“I knew what needed to be done,” she says, sitting up a little taller. “Either I stay here and fight my case, or I take my life. Transitioning was that important for me.”

Shanaya near her home in Newtown, Sydney (Photo by Ken Leanfore for Rolling Stone)
The average time refugees spend detained at Villawood is 16 months. Shanaya was released in six after her second application for a refugee visa on medical grounds was granted. Immigration staff at the detention centre were able to acknowledge the needs of a trans person, and agreed she was safer in Australia.
She moved in with Christian couple Trevor and Judy, who worked closely with asylum seekers through the Detention Centre. The couple introduced her to the Newtown Mission church and its Pastor, Andy, who became the first friend she ever came out to.
“I said, ‘If I tell you, I think you’re going to hate me’,” Shanaya recounts.
“He said, ‘Trust me child no matter what you tell me, my love for you, Jesus’ love for you, will never go away. It will always be the same’.”
Pastor Andy remembers it well too: “I wanted Shanaya to feel supported and not condemned by her fellow Christians,” he says.
“I find the whole debate and interaction between the Australian press, Church and the LGBTQI+ community to be generally very hateful and unproductive from all sides,” he adds. “A bit like people in fortresses firing cannons at each other. As somebody who is seeking to bridge the gap, I feel as if people on both sides need to leave their fortresses and get to know and relate to people who differ in their opinions and lifestyles.”
The Problematic Past and Present of Transgender Australia
If every coming out conversation was like Shanaya’s, perhaps more people would believe in God, perhaps advocates who lobby for trans and gender diverse rights wouldn’t be necessary, and perhaps trans people in Australia wouldn’t be nearly 11 times more likely to attempt suicide than the general population. Perhaps we wouldn’t have needed extensive research to uncover 15 transgender hate crime murders over the last 40 years.
In reality, Shanaya’s story of understanding from immigration officers and Sydney’s Christian community is the anomaly. The history of transgender people in Australia is highly contested and fraught with problematic provisional rules. In NSW, only those who have had genital reconfiguration surgery are protected by anti-discrimination law, but under the definition of ‘transsexuality’. In Western Australia, only those who have obtained a gender recognition certificate are protected under the ‘gender history’ provisions.
“Until 2014 every jurisdiction required trans people to have medical interventions to change their birth certificates, and in every state or Territory except WA it had to be gender affirmation surgery.” – Dr Noah Riseman
According to historian Dr Noah Riseman, there have been pushes to update the definition for transgender people in some states, but they haven’t all been passed in parliament. Dr Riseman’s research focuses on the social history of marginalised groups in 21st-century Australia. His work found that in NSW and QLD people must have sterilising surgery to change their birth certificates, and in WA they must have some medical intervention and also appear before a Gender Reassignment Board.
To update the gender marker that is recorded by institutions and organisations across Australia, many trans Australians have been forced to have sterilising genital surgeries in order to update their birth certificate. These laws still operate today in NSW, QLD and WA.
“There’s safety issues involved with that,” says Dr Riseman. “If Shanaya was pulled over by the police and they look at the ID and see Mr, they might treat her with respect, they might not.”
One of most problematic parts of these Australian laws is the assumption that all trans people want affirmation surgery. For some, fluidity is key to their gender identity. The trans community, lawmakers and the medical sector have long been divided. In the Northern Territory the anti-discrimination law still uses the outdated word ‘transsexual’ despite pushes to update the law. And until the late Eighties, trans people weren’t even allowed to change their birth certificates at all.
Much of the argument against trans people affirming their gender in this way is plagued by the thinking that if a person’s birth certificate can be amended based on their own sense of identity, this could negatively influence the fabric of society. However, at time of publishing there isn’t any evidence to suggest that is the case.
Two Steps Forward, One Step Back
It’s not as if being transgender is some new shiny subculture here to change up the status quo. Gender affirming medicine can be traced back through history, including to the early 19th century, during which Magnus Hirschfeld’s Institute for Sexual Science in Berlin became a focus for hormonal modifications. Hirschfeld, a gay, Jewish physician, later fled Berlin when the Nazi regime came to power. In fact, one of the Nazi’s first book burnings comprised of the sexual science books he was using to treat trans women using estrogen.
Over in the UK, between 1930 and 1950, British surgeon Archibald McIndoe constructed over 60 vaginas. And let’s not forget Danish artist Lili Elbe (played by Eddie Redmayne in 2015 film The Danish Girl) who underwent a series of treatments in the Thirties to reconcile her female self.
In the Forties, Irish medical student and trans man Michael Dillon became the first known person to use testosterone for the purpose of gender affirmation. For Lili Elbe, Michael Dillon, and even Olympian Mark Weston, who had affirmation surgery in 1936, each needed to remove their former identity to survive. For others, surgery isn’t necessary.
Life as a trans person can be an unsupported and unregulated path. It’s been a ‘two steps forward one step back’ approach. The medical and surgical practices in the Seventies, in Sydney especially, left a lot to be desired. Dr Riseman’s research found that trans people were regularly botched whilst undergoing gender affirmation surgery due to surgeons not being trained properly. One of his interviewees told him a story of a deceased trans friend who was “absolutely butchered” by the surgeon.
“She was left lying in blood and ended up with a fistula (an internal sore that never heals) that every so often would go off like a volcano and would leave a boil that would damage her genitals and would burst,” he says, reading from his notes of the interview. “There would be rancid pus coming out of it. She lived like that for years until she took her life.”
While genital surgeries today are amongst some of the most advanced and innovative in the world, the path to undergo them is still stuck in the past, and the heavy burden trans people carry mentally overall is directly linked to how they are treated.
Medical Intervention Is “Invasive and Humiliating” in Australia
The transgender paradigm shift of the Nineties might have brought about a freedom of gender definition, but just as culture moves faster than the laws which govern it, Australia hasn’t been able to keep up with the needs of its transgender population.
The process to have genital reconfiguration surgery in Australia is difficult to say the least, and in essence privileges a particular kind of transgender person: someone with access to between $8,000 and $200,000 depending on the kinds of surgical affirmations they’d like to make – most gender affirming surgeries are not covered by private health insurance or Medicare.
Following GP visits with doctors who have limited guidelines on how to engage with or prescribe for transgender patients, the path to surgery is a series of waiting rooms and consultations with people who, by many accounts, pathologise transgender as a mental illness. In Australia, the current path involves hormone replacement therapy (an indefinite expense); visits with endocrinologists and psychiatrists for pre-op evaluations; and a visit to two doctors and a Justice of the Peace (yes, really), to gain a new birth certificate in the states which allow it.

Teddy Cook, Manager of Trans & Gender Diverse Health Equity at ACON. (Photo by Ken Leanfore for Rolling Stone)
Teddy Cook, Manager of Trans and Gender Diverse Health Equity at community health organisation ACON, is a staunch ally of the LGBTQI+ community. Sitting in the ACON boardroom in Sydney, Cook speaks with the kind of impressive academic consideration usually reserved for public figures. Cook believes there should be no requirement for medical intervention for a simple record like the birth certificate to be updated.
“The process in NSW is invasive and humiliating,” he says. “Not only are adults and children forced to have surgical interventions they might not want, they also need to have this examined by two doctors to update the gender marker listed on a birth certificate.
“A statutory declaration is signed by two doctors confirming you have undertaken the requisite surgical intervention. Then each of those doctors need to go and see a notary or justice of the peace to witness the signatures. Some doctors even bring a JP into the room for these examinations. None of this is okay but it is the current law in NSW. Tasmania has led the way with recent birth certificate law reforms though and NSW must be next.”
If Cook sounds embittered by the current system, that’s because he is. Cook began affirming his own male gender 15 years ago, and having led the release of this year’s TransHub platform for all trans people, allies and clinicians in NSW – and as the Board Director of the Australian Professional Association for Trans Health (AusPATH) – he speaks from personal and professional experience.
“The social, medical and legal steps I’ve taken to affirm my gender aren’t the things that have made me a man. I’ve always been male – even if those around me couldn’t recognise that,” he says. “But they have helped me live in this society as a man.”
Cook says the oft-used trope of feeling ‘born in the wrong body’ not only gives the medical sector reason to pathologise transgender as an overall misprint in humanity, but it negatively feeds into the psyche of trans people. “I don’t know if trans people are born in the wrong body or if society traps them in the wrong body,” he says assuredly.

(Photo by Ken Leanfore for Rolling Stone)
Access is one of the biggest hurdles here in Australia. There is limited or no Medicare funding for the vast majority of gender affirming surgeries, and with cost being the major barrier, many patients expect to never be able to afford surgery in their lifetime.
“We see people who are affirming their gender a little later on in life, who may have had a successful corporate career, who then need to spend their savings on surgeries,” says Cook. “Many people apply for a compassionate early release of superannuation so that they can access the surgical intervention that they seek.”
There is one program for subsidised gender affirmation surgery in Australia. Monash Gender Clinic in Melbourne does receive public funding from the Victorian Government but it’s chronically underfunded. Between 1987- 89 they had to stop doing surgeries altogether and when funding resumed it allowed just 10 surgeries per year, despite waitlists over 35 people.
Back then, a precedent was set: successful patients for the subsidised surgery scheme were only granted surgery after a recommendation from a psychiatrist. This hasn’t changed in over 30 years.
Due to psychiatrists acting as gatekeepers to surgery, some trans people have found that by not adhering to stereotypes and clichés related to their affirmed gender they were denied altogether. This started in the Eighties and has remained one of the vicissitudes of trans history.
“You had to present this very stereotypical, Fifties housewife way of being female,” says Dr Riseman. “If you were gay then that wasn’t right. There was a very particular mindset.”
Teddy Cook says that even now, trans people are forced to relay rehearsed histories in order to receive surgical permission.
“Trans people and our community have taught each other the script that you need to say. You have to shell out lots of money, you have to perform a particular variety of who you are to get what you need,” he states matter-of-factly. “There is certainly nothing therapeutic about that process.
“There is something quite horrific about people in power, that have the power to approve something about your own body, when they want you to be a particular variety of way.”

Dr Michelle Guttman-Jones. (Photo by Ken Leanfore for Rolling Stone)
Shanaya is yet to have her surgery, but she plans to use the early release of her superannuation. I ask her what the visit with her psychiatrist was like when it came to requesting surgery. Unfortunately, her experience followed those who had gone before her, even decades ago.
“He liked that I had my nails done,” she says, smiling.
“The psychiatrist asked me, ‘What about dressing up?’ I told him I don’t think transitioning is about being dolled up. It’s about expressing yourself. I said there are lots of women nowadays who go out wearing jeans and a t-shirt. You don’t have to be in frilly dresses, you don’t have to have tonnes of makeup on your face.
“If I’m confident going out in society and saying, ‘My name is Shanaya and I’m a woman’ – regardless of what I’m wearing – that’s what matters.”
The Invisibility of Transgender Health
Shanaya was never going to be a victim of circumstance; despite her experiences, she lives a life of gratitude in a world which largely refuses to acknowledge her gender. But is it any wonder trans advocates are suspicious of medical models and legislators?
Some fixes are easy, like requesting patient pronouns. Others are more complex, like the fact the current medications to treat trans people are listed by medical bodies as treatments for cisgender people. Meaning, the medications trans people use are for post-menopausal cis-women and cis-men with established testicular disorders and PBS, the Pharmaceutical Benefits Scheme, does not recognise gender affirming hormone therapy as an indication for prescribing hormones.
“That makes it difficult for GPs who don’t know what they’re doing,” says Dr Michelle Guttman-Jones, a Sydney-based GP with a specific interest in transgender health.
“They look up these medications and they see that these are for people with testicular disorders and this patient doesn’t have testicles so therefore this patient can’t have this medication,” she explains. “What the gender affirming doctors are doing is basically bending the rules and, at times, putting themselves on the line to treat their patients.”

The office of Dr Michelle Guttman-Jones. (Photo by Ken Leanfore for Rolling Stone)
Seated in her office in Newtown, she shows me a basic form for patients which is inclusive of trans and gender diverse patients. She also points to a sticker tacked to her computer which reads ‘my pronouns are she and her’ and smiles as if to say, ‘It’s not hard’.
But in a country currently debating whether a doctor could tell a trans patient they believe God made men and women in his image (re: the proposed Religious Discrimination Bill), she’s certainly not preaching to the choir.
“Transgender health doesn’t even exist to the government,” she says. “It doesn’t exist anywhere.”
Another tragic betrayal of humanity is where we see endocrinologists and psychiatrists become the gatekeepers of trans healthcare. A shocking 2016 study found only 20% of endocrinologists were “very” comfortable discussing gender identity and/or sexual orientation with their patients.
Dr Guttman-Jones says we don’t need endocrinologists for trans health. “GPs can do it, sexual health physicians can prescribe these medications,” she says. “You just have to care enough about it to learn how to do it.”
Dr Guttman-Jones compares the journey of gender affirmation to any other permanent body modification. “It’s the same as a tattoo. A tattoo is also a permanent body modification; but we don’t make people see a psychiatrist for that.”
Making the Transgender Tipping Point Count
The real experts in all of this are not the psychiatrists, it’s not the surgeons and it’s certainly not the lawmakers. It’s people who are transgender.
Trans culture may be experiencing a tipping point, but it’s no thanks to current legislation. It’s thanks to this important period of critique where the growing community is using its voice and its numbers. Right now, it’s unsafe for trans people to access healthcare and the laws surrounding it are as draconian as they are transphobic.
Right now, there are cultural competencies which could be updated. Similar to the competency guidelines that stop a male doctor examining someone wearing a hijab, basic cultural competency around trans health could easily be mandatory amongst medical professionals.
People like Dr Michelle Guttman-Jones and Teddy Cook are actively working to make trans health safe, and they have simple, but effective requests.
“I would like to see the depathologisation of the trans experience amongst the medical community,” says Dr Guttman-Jones. “I want doctors to see it as their role to facilitate gender affirmation rather than to ‘treat gender dysphoria’, which is not a disease or a mental health condition.
“I would also like to see the decentralisation of gender affirming healthcare,” she continues. “[…] I want it to be as easy to get your hormones from your GP as it is to get your blood pressure medication.”
“My hope is that we will start to see a rethink on how we situate things like gender dysphoria,” says Teddy Cook. “[…] I’d like to see a movement away from dysphoria and into euphoria, or into a space where our bodies are seen as normal, a perfectly normal human experience.”