Photo by Jill Levers
No longer relegated to the pages of Fear and Loathing in Las Vegas, psychedelic therapy substances are being considered seriously as effective treatments for mood disorders and addiction.
The guests stand in a circle digging their own graves. They’re forced to lie in them while people above scatter dirt over their prostrate bodies. Dappled sunlight filters through tropical vegetation while an ethereal figure standing in the centre rattles off platitudes in a thick accent. This is how one of the therapy sessions plays out in the recent fictional series Nine Perfect Strangers. The retreat owner Masha, played by Nicole Kidman, invites a select group to her wellness retreat and then has them drink psychedelic substances without their knowledge or consent. Unbeknownst to them, the guests start their day with a breakfast smoothie laced with psilocybin (magic mushrooms) and spend most of their time relaxing in the lush grounds of a Californian retreat. There’s the odd acupuncture session and the occasional group activity, but not much in the way of clinician-assisted therapy. The show flirts with the idea of psychedelic therapy, but, as you might expect from a drama based on a novel, it’s a far cry from reality.
There are currently plenty of scientific studies underway looking at treating mental disorders with the help of psychedelic substances. According to an article in the Australian & New Zealand Journal of Psychiatry, in 2021 there were approximately 100 clinical trials around the world using psychedelics. These are not tropical getaways for the wealthy, but rigorous evidence-based trials that could change the way we look at mental health treatment.
Scientists and doctors are experimenting with substances commonly considered recreational drugs, rather than seen as medicines. The trials include the use of psychedelics like LSD (acid), ayahuasca, and psilocybin. Even party drugs like MDMA and ketamine, which aren’t strictly psychedelics, are being used to treat serious disorders. While most of these are prohibited substances in Australia, they’re being used increasingly in research. Ketamine has even been approved in Australia to treat Major Depressive Disorder where other medications haven’t worked. And it’s not just depression these treatments could help. There’s hope that psychedelic therapy could be used to treat generalised anxiety disorder, alcohol and drug dependency, tobacco dependency, and even body dysmorphia.
Despite the sobriquet given to psilocybin, these substances are not being administered as a magic cure. It’s not as simple as drinking a smoothie and relaxing poolside at an expensive retreat. Taking psychedelics allows patients to experience themselves in a different way and creates an environment for them to confront repressed traumas. When paired with intense and individualised therapy, evidence suggests this can lead to a significant improvement in some psychiatric disorders.

Dr Jerome Sarris. Photograph by Saskia Palmer-Sarris.
Launched in 2021, the Psychae Institute is an Australian centre which specialises in psychedelic medicine and research. One of its founders, Dr Jerome Sarris, who describes himself as a “tele and strat playing tragic” and has an impressive collection of custom guitars, is one of the world’s leading experts on medicinal plants. He has conducted extensive research on ayahuasca, a psychedelic combination of two plants consumed as a ‘tea’ and used by Indigenous people in the Amazon basin for centuries. According to Dr Sarris, when it comes to taking ayahuasca, “you’re forming new connections in your brain while dampening others… you’ve got all these different interrelations biologically, but then you’ve got the psychological experience”.
Dr Sarris makes it clear that it’s still early days, but the studies he’s been involved in have indicated ayahuasca’s enormous potential. “It’s a new frontier, and we’re only just finding out what the particular mental health benefits can be, but our data was really quite compelling, showing that people who did report ayahuasca use did have a dramatic reduction in depression, in depressive symptoms, also a reduction in anxiety symptoms… a strong effect on reducing trauma, as well as alcohol and substance use.”
“It’s a new frontier, and we’re only just finding out what the particular mental health benefits can be.”
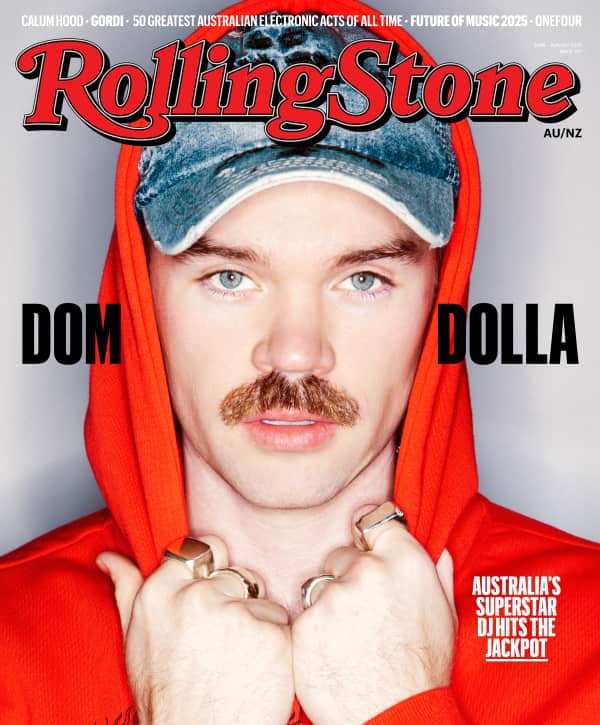
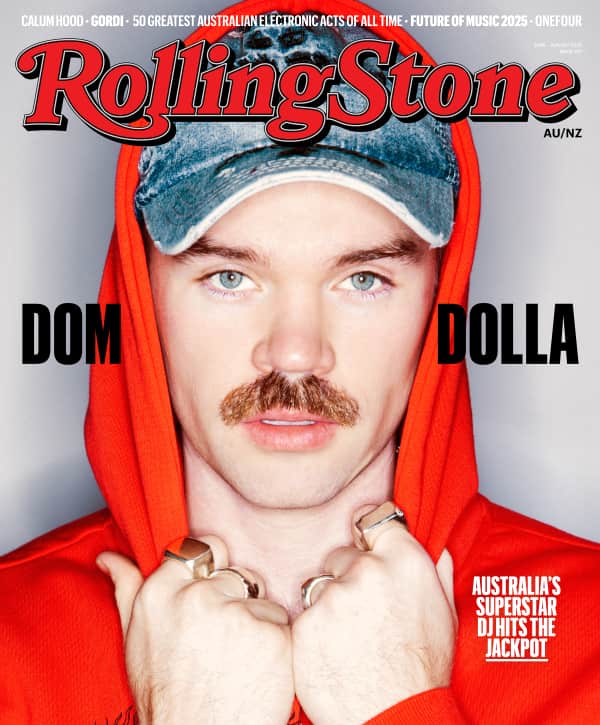
Love Music?
Get your daily dose of everything happening in Australian/New Zealand music and globally.
Dr Sarris believes that we’re in the middle of a “mental health pandemic”, and his goal is to provide better healthcare for patients in a safe environment. While his current focus is on treating mental health disorders, he doesn’t rule out future research into whether psychedelics could be used to help us tap into our creativity. “In later times I anticipate that attention will turn more formally towards the effects on human consciousness,” he explains. “This can be applied to address broader societal and existential issues, and to enhance psycho-spiritual growth, creativity, and innovation.”
Dr Susan Rossell, a specialist in cognition at Swinburne University of Technology, is running a study out of Melbourne using psilocybin to treat major depressive disorder. “We often refer to (psilocybin) as resetting the brain or opening up the brain to new experiences… getting rid of that roadblock that can often be there for people with serious mental health disorders.” She sips out of a pink mug with a zebra on it while she talks through her protocol. Dr Rossell is trying to “perfect the ingredients” with varying combinations of dosage and therapy. First, the therapist establishes a rapport over several sessions to better understand the patient’s triggers and how they approach their depression. Only then are they invited back to take the psilocybin.
A typical treatment day starts early in the morning as the dose can last for six to eight hours. The patient spends this time in Dr Rossell’s clinical suites, which are nothing like the sterile office you might find at your GP; they’re filled with plants, pictures, paintings, and a sofa to recline on. Music plays while the patient occupies themselves with crafts or flicks through the pages of art books. While in the safety of Dr Rossell’s suites, the therapist monitors the patient to reduce the possibility of a negative encounter. The therapist might gently guide the patient through their experience but there’s not necessarily formal therapy during the dosing session. As Dr Rossell explains, “The real work starts a couple of days afterwards, with their mind opened up, then they start to work on the issues that have been identified prior to the therapy.” Dr Rossell’s trials are still ongoing but results from global studies suggest that psilocybin can be an extremely effective treatment against major depressive disorder. “One of the reasons it’s becoming incredibly popular… is that there are more people recovering from psilocybin-assisted psychotherapy than we’ve seen with any other new intervention in the last 20 years. There’s a really high recovery rate of around 40-50%, which is unheard of with any other (treatments).”

Maloka-Nimea Kaya Healing Center Lodge in Peru. Photo by Jill Levers.
To understand the experience from another perspective, I interviewed someone who has participated in multiple ayahuasca ceremonies. Rachel (whose name has been changed to protect her anonymity) is a successful Australian professional in her thirties, well-presented, with a manner that oscillates rapidly between pensive and ebullient. When the camera feed connects, she’s sitting outside on a balcony in the Sydney sun, with a dog spread lazily on the floor behind her. She speaks animatedly about her experiences at an ayahuasca centre in Peru. “It’s like spiritual open-heart surgery,” she says half-smiling, half-terrified.
“It’s like spiritual open-heart surgery.”
At the centre Rachel visited, located in the lowland jungles of the Amazon, the guests participate in night-time ceremonies where they sit in a circle while local shamans sing “healing songs”, before they drink the ayahuasca tea—triggering the psychedelic experience. Rachel refers to it as “medicine” and gives it the pronoun “she”, as if the substance has a consciousness of its own. Some people believe the medicine speaks to you directly. “Sometimes she’ll keep repeating the message to you,” Rachel says. The medicine shows you what you need to improve your life and your relationships. Rachel looks serious, “the message is very clear… you know what you have to do, but whether you’re willing to do the work is a different story”. According to Rachel, the experience can be different every time you drink the tea, and it varies from person to person. Sometimes the ceremony might last for a few hours and sometimes it can go all night. Some people cry with abandon, others throw up, purging themselves physically and psychologically.
While Rachel’s first few times were “mild and gentle”, she describes her fourth experience as a “boom.” With a slight giggle she explains, “It’s like I got punched in the face and pinned down and couldn’t move. It was just like I was obliterated.” Given Rachel compares the experience to a psychological bashing, you might wonder why people would put themselves through it and whether it’s actually worth it. While Rachel clarifies that she’s not rushing back to do it again, she explains that her life “has changed like you would not believe as a result of having done it… home, work, relationships, family”. She gained insight into her relationship with her mother that allowed her to understand her in a way she never has before. It’s hard to comprehend the effects without experiencing them firsthand, and possibly even harder to put into words—although many describe undergoing some kind of mystical experience. As Rachel put it: “All I can see is energy.”
The centre Rachel attended is somewhere where “people in their early 20s to people in their 60s” come from all over the world to join. While it’s not a formal clinical environment, there are facilitators who are responsible for the guests’ safety. Everyone has to provide their medical background to check they’re suitable candidates. Shamans are also present and give the participants a “flower bath” and something to eat after the ceremony, which helps ease them back into reality. Group sessions are facilitated after the ceremonies to work through the experience as a collective. There are also rules which require participants to abstain from junk food, partying, and sex in the weeks before and after.
There are also rules which require them to abstain from junk food, partying, and sex in the weeks before and after.
The whole thing isn’t exactly cheap. Rachel paid $2,000, and some places charge up to $10,000. Ayahuasca retreats have popped up throughout the world and range from camping to luxury resorts. Costa Rica’s well-known Rythmia also offers a health club, gym, spa, massages, mud baths and a swimming pool. On top of the fees, you still need to factor in the cost of flights if you’re coming from abroad. This may not seem like an unreasonable amount for food, accommodation, and a potentially life-changing experience, but the price point puts it out of reach for most. On the other end of the spectrum, you can find people selling ayahuasca in bottles on the side of the road for those who want to risk taking it without any supervision or guidance.
Far from the Amazonian jungle and the streets of Costa Rica, people are using psychedelics at home, alone or with friends, to self-medicate. According to Dr Adam Winstock, a consultant psychiatrist who runs the Global Drug Survey (GDS), while there has been a slight dip in usage because of COVID-19, there has been a noticeable upward trend in psychedelic use globally over the past few years. Some people are even switching from their prescribed medications and turning to psychedelics instead. “There are huge risks with self-diagnosis,” Dr Winstock warns. “I worry about the most vulnerable in society either being exploited by dodgy people or taking treatment into their own hands.”

Maloka-Nimea Kaya Healing Center Lodge in Peru. Photo by Jill Levers.
Microdosing, which involves taking such a small amount of a psychedelic substance that no hallucinogenic effects are felt, is a trend also seeing an increase in popularity. Anecdotally, people claim that microdosing increases creativity and general sense of wellbeing, but there aren’t sufficient scientific studies to support this. Dr Rossell pauses when questioned on this: “Lots of hearsay, not a lot of research.” Because these substances are still illegal in most countries, microdosing occurs without direction from medical professionals. You can find guidelines for microdosing all over the internet, but these substances can have very individual effects, and what may be a microdose for one person may not be for another. Doctors warn that people sometimes mistakenly take more than a microdose, sending them into an unsettling and unexpected space between high and sober.
For some people, these substances are so strongly associated with recreational drug use that they can’t entertain the possibility of other applications. Dr Winstock explains how our understanding of substances can often be reductive: “We like very clear dichotomies, good drugs and bad drugs… and it’s not that simple.” Attitudes do appear to be changing albeit slowly; the Australian Government for one has been offering grants to fund research into psychedelics through the Medical Research Future Fund.
“We like very clear dichotomies, good drugs and bad drugs… and it’s not that simple.” – Dr Adam Winstock, Global Drug Survey
While things may look promising, we face years of research and trials before these treatments become widely accepted medical practice. Whether they will be accessible to everyone is yet to be seen. Weeks of intensive therapy requires a lot more resources than taking a pill, and a whole generation of medical professionals will need retraining. Dr Monica Barratt, a social scientist who has been working in drug policy for twenty years, highlights that “psychedelics tend to be used by people who have a bit more privilege in society”, and that could be why they have less stigma than other illicit substances. Will psychedelic therapy become something reserved only for the wealthy? That depends on how governments and insurance companies around the world respond. Although, as several people interviewed for this article pointed out, the cost of six to ten weeks of intensive therapy is a lot less than the public health cost of treating someone with a lifetime of addiction or a debilitating mental health disorder.
For many of these substances, addiction is not an issue. They are self-limiting because you build a tolerance relatively quickly. Dr Winstock says that he has never seen anyone “seek treatment for MDMA or psychedelic dependence”. Everyone interviewed agreed that more research is required, and the primary concern at this point is ensuring the safety of potential patients. In the meantime, perhaps we need to remain open to the idea that these substances are good for more than just getting high. As Dr Winstock explains, “The difference between what we call a drug and a medicine is down to who you get it from, and why you use it.”
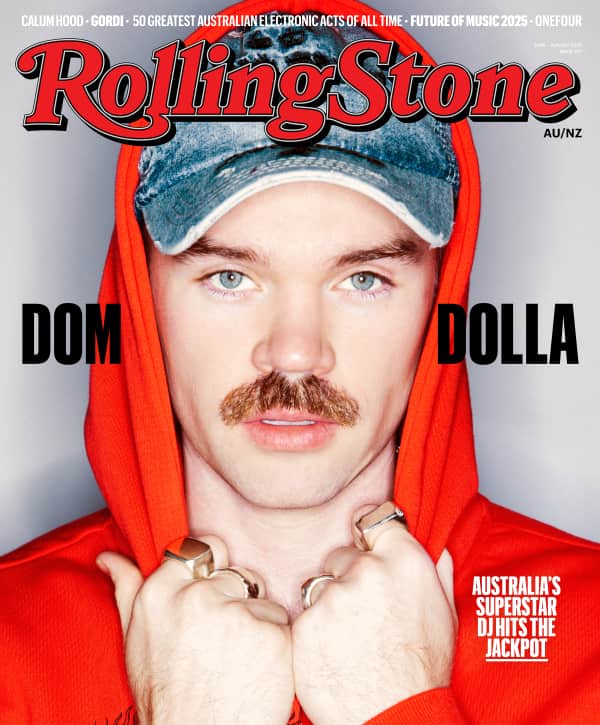
This article features in the March 2022 issue of Rolling Stone Australia. If you’re eager to get your hands on it, then now is the time to sign up for a subscription.
Whether you’re a fan of music, you’re a supporter of the local music scene, or you enjoy the thrill of print and long form journalism, then Rolling Stone Australia is exactly what you need. Click the link below for more information regarding a magazine subscription.