Imagine, if you can, life as it was a few months ago. Shopping for groceries without nervously eyeing anyone who creeps within six feet of you. Sitting down for dinner at a restaurant and actually enjoying the crowd. Watching live sports. These ho-hum aspects of everyday life are now the stuff of fantasy, reminders of a way of life the world is growing more and more desperate to reclaim. A beer in a bar with a friend feels as exotic as a daiquiri on a South Pacific beach.
A more pressing fantasy to fulfill is the one in which hundreds of Americans aren’t dying on a daily basis from a virus the scientific community still doesn’t fully understand. Unlike some other nations, the U.S. has been unable to contain the spread of the virus, which means the development of a vaccine is likely the only way to reclaim any semblance of normalcy. Desperation for one has led to an unprecedented mobilization in which governments, scientists, and the pharmaceutical industry have trained their energy on bringing one to market in record time.
So when will a vaccine be available? Why, with so much interest and resources funneled into the cause, are researchers unable to develop one faster than many are projecting? Why is there so much uncertainty about when the population will be able to receive inoculations, and some pandemic-mutated version of life as we once knew it will be able to resume?
When President Trump was first asked how long Americans would have to wait for a vaccine on March 2nd, he threw out “three or four months” before deferring to Dr. Anthony Fauci, the nation’s leading infectious-disease expert. Fauci clarified that it “is going to be, at the earliest, a year to a year and a half” before a vaccine is deployable, “no matter how fast you go.”
Just over two months and 80,000 dead Americans later, the Trump administration is promising a vaccine will be available to the American public by the end of the year, the result of an initiative dubbed “Operation Warp Speed.” Fauci is still sticking to his 12-to-18-month time line. “I think it is more likely than not that we will” get a vaccine within a year or two, he told senators during a hearing last Tuesday, citing the progress made since the effort began. “It’s definitely not a long shot.”
The progress so far has been encouraging, if not remarkable. Bringing a vaccine candidate for a novel virus through clinical trials typically takes years, usually many of them, but in just four months since COVID-19’s genetic sequence was determined in January, a handful of candidates have entered clinical trials. The most promising among them are expected to wrap up human testing by the end of this year. New technologies are being harnessed, companies and governments that typically compete are now collaborating, and billions of dollars in funding has been made available. These are all promising signs, but they don’t guarantee a vaccine will be available anytime soon. The time line remains the biggest unanswered question.
According to a 2013 paper by researchers at the University of Rotterdam, in the Netherlands, the average vaccine development time line is 10.71 years. The record is four years, how long it took to develop a vaccine for mumps in the Sixties when regulations weren’t as stringent. Meanwhile, researchers have been working on an HIV vaccine for close to 40 years. Most experts ballpark the range of potential time frames anywhere from five to 20 years.
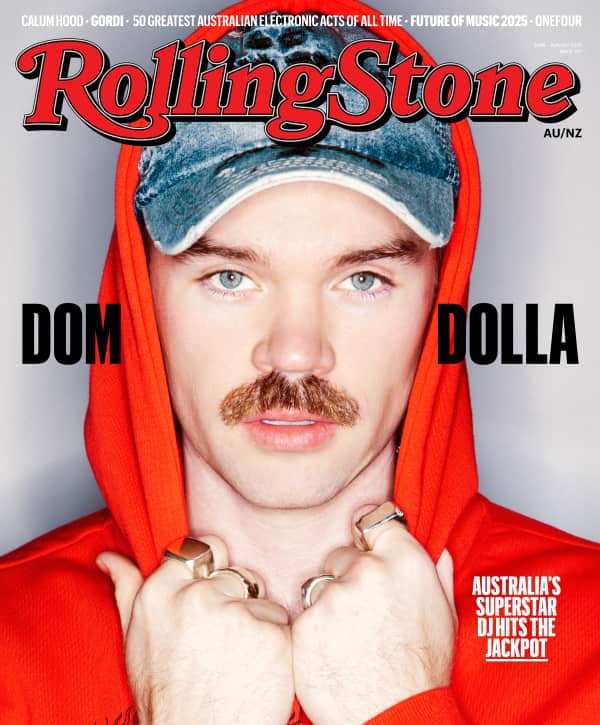
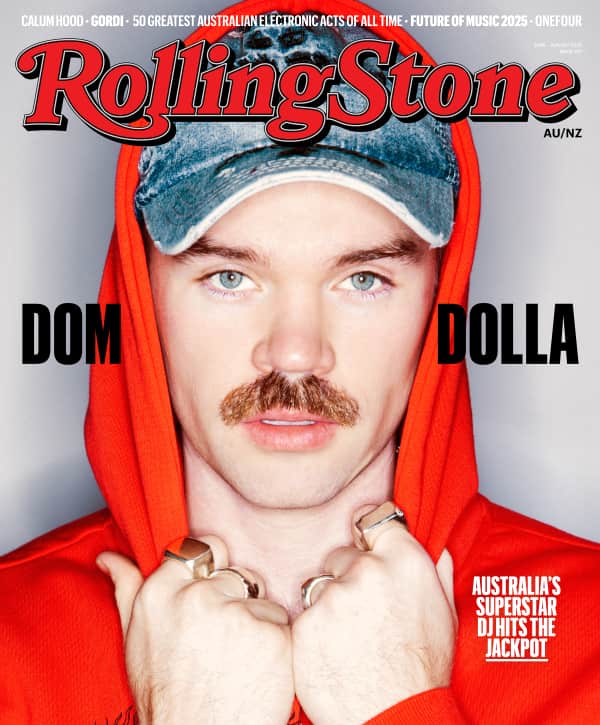
Love Music?
Get your daily dose of everything happening in Australian/New Zealand music and globally.
While these experts allow that a COVID-19 candidate could be licensed — not to mention manufactured and distributed — within 12 to 18 months, they also note that it is highly unlikely. “It’s more than just the optimistic side of the spectrum,” says Dr. Peter Hotez, dean of Baylor’s College of Tropical Medicine. “It’s the unprecedented side of the spectrum. That’s the part that concerns me. We’ve never done it. It doesn’t mean it’s impossible and we’re not trying, but it’s never been done.”
Rolling Stone spoke with experts to get a better understanding of the complicated, delicate process of developing a vaccine that will be injected into the arms of hundreds of millions if not billions of healthy people, and what the quarantined masses can expect from the effort in the coming months.
Research
One of the reasons we could see a vaccine within the next year or two is a dramatically shortened research runway. Scientists typically need years to study a virus and secure funding to develop a vaccine candidate. The latter is especially difficult. “One of the reasons you don’t see a lot of [investment] in this space is because the time horizons are long, the risk is high, and most things don’t advance,” Hotez says.
Hotez and his longtime collaborator Dr. Maria Elena Bottazzi spent nearly 20 years developing a vaccine for SARS-1, which infected hundreds in Asia and Canada in the early 2000s, but ultimately had to put it on the shelf before entering clinical trials because they ran out of funding. But the time Hotez, Bottazzi, and others spent researching coronaviruses like SARS and MERS has given scientists a huge head start in the race to develop a vaccine for SARS-Cov-2, the novel coronavirus that causes COVID-19.
“Our SARS vaccine went through a very robust series of tests to evaluate purity, quality, functional ability, induce the right immune response, and ensure safety,” says Bottazzi, who along with Hotez is now working to develop a COVID-19 vaccine. “You can extrapolate a lot because these viruses are very similar.”
This base of knowledge has emboldened scientists to forge ahead where in the past more research may have been warranted. Though this may increase the likelihood of failure, it’s a worthwhile risk considering the sheer number of players in the game. There are more than 115 vaccine candidates currently in development. Only a few of them need to succeed to cover the global need. “If you really want to get to that time line of one year to 18 months, it means simultaneously advancing a lot of candidates forward,” Hotez says. “It’s really the safety testing that is going to take longer than anything else.”
Testing
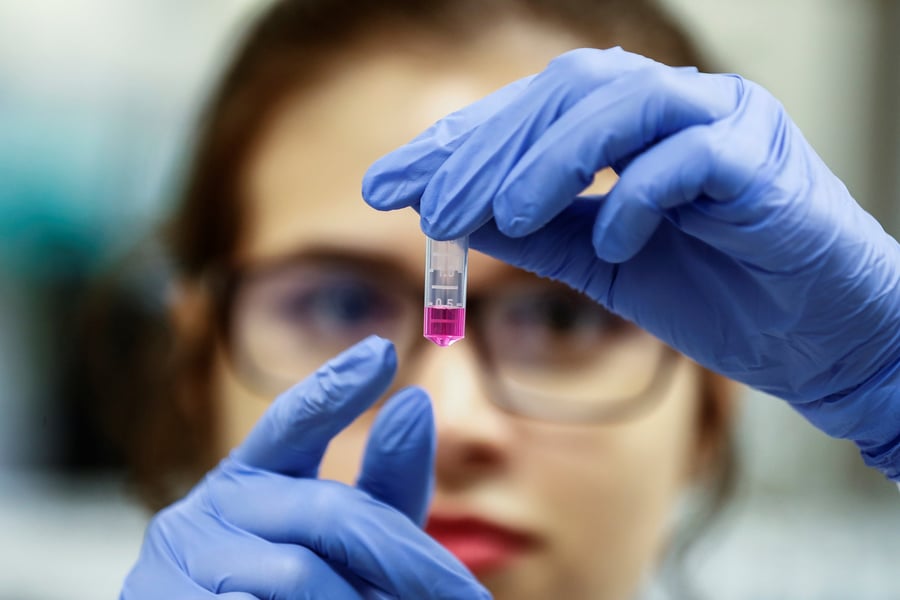
Testing a vaccine candidate typically involves running it through preclinical trials in which it is tested on animals, followed by three phases of clinical trials, starting small with a few dozen human subjects before broadening to tens of thousands.
Researchers working to develop a COVID-19 vaccine want to compress this process, which invariably takes years of trial and error, into a few months. Testing is being done on humans and animals concurrently, and less time will be taken to study the results of each phase of human trials before moving onto the next. As Hotez puts it, developers have been charged with trying to do things “in parallel, rather than serially.” For example, Moderna, a biotech company that has received $430 million in federal funding, recently announced plans to begin Phase III trials in “early summer.” Meanwhile, they haven’t even entered Phase II yet, and only began Phase I in March.
As Fauci noted while speaking to senators last Tuesday, at least eight COVID-19 vaccine candidates have entered clinical development. Moderna is one of them, and on Monday the company announced their candidate appears to be safe and to have generated an immune response in the eight people it was tested on in March. The company has been a favorite of Fauci, who praised its progress while speaking to senators. But it’s also using a technological platform — messenger RNA, or mRNA — that has never yielded a licensed vaccine. “There is no mRNA vaccine like this yet,” says Dr. Rino Rappuoli, chief scientist at GlaxoSmithKline, one of the world’s leading vaccine manufacturers. “We don’t know how effective it’s going to be. It’s kind of an unknown.”
There are other risks to accelerating the testing process. Experts have cautioned about the potential for a vaccine to make the disease worse, an issue that emerged in animal testing for SARS-1. COVID-19 also has a relatively high asymptomatic infection rate (between 20 and 40 percent), which means a larger testing pool is ideal, and the likelihood of re-exposure, which is far greater than that of SARS-1, means a longer-term evaluation period is preferable. Unfortunately, it’s not an option. “When you have an emergency, you can change the ratio between the risks that you want to take to the benefit you’re going to gain,” Rappuoli says.
Researchers are confident the sheer number of candidates spread across different platforms will result in a variety of safe, effective options that can satisfy the global need — even if the majority of them fail. “We have multiple candidates and hope to have multiple winners,” Fauci said on Tuesday. “In other words, [we’re taking] multiple shots on goal.”
This doesn’t necessarily mean anyone is going to score. The same University of Rotterdam study that set the average vaccine development timeline at 10.71 years also found that only six percent of vaccines that enter clinical trials go on to enter the market, and this is after years of research, approvals, and testing. The harried nature of the race to develop a COVID-19 vaccine only increases the likelihood any given candidate will fail.
Licensing
After a vaccine candidate makes it through clinical trials, it must be licensed by a regulatory agency. In the U.S., it’s the Food and Drug Administration, which typically takes around a year to license new drugs. This isn’t a typical situation. “When you are under pressure like now, the regulatory agencies that usually take a long time just to respond to you, now you can talk to them every day,” Rappuoli says. “They are very eager to accelerate the global collaboration between vaccine developers, pharma, and regulatory agencies.”
This should be easy then, right? More or less, but some worry it may be too easy. The FDA will be under a tremendous amount of political pressure to license a vaccine candidate, and its commissioner, Stephen Hahn — whom Rolling Stone recently highlighted as one of the four men responsible for America’s failure to respond to the coronavirus — doesn’t exactly inspire confidence. “There was a moment when Donald Trump said the FDA was working with them,” says Dr. Paul Offit, director of the Vaccine Education Center at the Children’s Hospital of Philadelphia and member of the FDA’s vaccine advisory committee. “That worries me.”
Also of concern to Offit is the prospect of the FDA forgoing the approval process entirely. “I worry they’re going to use Emergency Use Authorization to get around the FDA,” he says. “I think that would be a mistake. I really do. Although we see regulation as burdensome, you want the FDA to regulate these products. You want someone to take a long hard look at what the data are before they license it for use in this country.”
It wouldn’t be the first time an unapproved vaccine was deployed. In 2014, an Ebola vaccine still in clinical trials was given to front-line workers in West Africa. The experiment was a success and the vaccine was ultimately approved in 2019, but by the time it was first administered, researchers had been studying its potential effects for years, not months. “There’s no time to do that in-depth of a functional evaluation,” Bottazzi says. “The FDA should follow due process based on evidence, but they’re also put in the very not normal position of having to do it fast, and they may [not be able to look at] the full study of evidence.”
The decision over whether to license a vaccine immediately will hinge on a risk-benefit analysis. How dire is the immediate need for those most at risk? How easily could the vaccine be manufactured and distributed to them? To what extent are alternative treatments an option?
As with every aspect of this accelerated development process, scientists are having to make such determinations on the fly. Hotez has faith in the FDA to make the right decisions, but in the end it’s hard to know what to expect because the situation is so unprecedented. “[The FDA] tends to insulate themselves pretty well from all the hype, and they tend to look at things without bias,” Hotez says. “They’re really good scientists trying to think through this so I don’t think they’re going to be swayed. But who knows what’s going to happen.”
Manufacturing and distribution
Developing a safe and effective vaccine in a few months would be one type of miracle. Manufacturing hundreds of millions of doses of it, and then distributing those doses equitably, may be an even greater challenge that will require an unprecedented level of international collaboration, both among nations and between governments and private interests.
First and foremost, it’s going to require establishing infrastructure to produce hundreds of millions (if not billions) of doses of specific vaccines before they can be proven safe and effective. Johnson & Johnson, which has received nearly $460 million in federal funding, is already working on operationalizing factories, as are Moderna, Pfizer, and other developers near the front of the race. Bill Gates announced on The Daily Show recently that his foundation is contributing billions to help seven unnamed companies that are developing vaccines to ramp up their manufacturing in advance.
“We will be producing vaccines at risk,” Fauci told senators, “which means we will be investing considerable resources in developing doses even before we know if any given candidate or candidates work.”
A recent report from Politico outlined several of the complications with scaling the production of a vaccine, including a shortage of the types of glass and stoppers needed to construct vials, which could cause delays down the line. Once manufactured, the vaccine doses need to be stored and transported in a controlled temperature. This is just in the U.S. “Everything has a challenge because you’re using different techniques and machinery,” Hotez says. “Things are done differently in India than they are in Brazil.”
Then there’s distribution. “Assuming some of these vaccines will get licensure in a very optimistic scenario, then the question is how many doses will be available,” Rappuoli says. “A million? 10 million? 100 million? A billion? How are you going to make this decision? Where should the vaccines go? This is going to need a lot of collaboration globally. Otherwise, countries are going to be very conservative and say they need it for themselves.”
It could depend on where the first vaccines proven safe and effective originate. If they’re produced overseas, the U.S. could have trouble getting them. One of the most promising candidates in being developed by a group at Oxford University, which hopes to have a few million doses ready by September, but because pharmaceutical companies typically demand world-exclusive rights, they’ve yet to work out a deal with an American manufacturer. At the same time, Sanofi, the French pharmaceutical giant developing two candidates in a collaboration with GlaxoSmithKline, has said the U.S. will have first dibs because it has “invested in taking the risk,” as the company’s CEO recently told Bloomberg.
The potential for a global competition over vaccine doses is why Fauci and others have stressed the importance of putting a diversity of candidates through trials. “No single vaccine or vaccine platform alone is likely to meet the global need, and so a strategic approach to the multipronged endeavor is absolutely critical,” he wrote along with three other top scientists in a paper published this week in Science.
They concluded by emphasizing the need for cooperation: “Cost, distribution system, cold chain requirements, and delivery of widespread coverage are all potential constriction points in the eventual delivery of vaccines to individuals and communities. All of these issues require global cooperation among organizations involved in health care delivery and economics.”
So, how long will it be until a COVID-19 vaccine is available to the general population?
No one really knows. There are so many variables involved in the production of a vaccine, and the mad dash to develop one in response to COVID-19 is so unprecedented that there is no way to predict when, how, or by whom a scalable candidate will emerge.
What most experts agree on, however, is that the 12-to-18-month time frame floated by Fauci is on the more optimistic side. “When you say 12 to 18 months, I don’t see how you can possibly learn everything you need to know in that time,” Offit says. “I understand that we’re panicked about the virus, but I worry corners might be cut. I honestly think that if everything went perfectly you could make this vaccine in five years.”
Rappuoli believes it is “technically possible” to have a vaccine ready in 12 to 18 months, but acknowledges that getting one licensed in that time frame — not to mention manufactured and distributed — is probably a best-case scenario. “I think we can shorten the time line,” he says. “How much we can shorten it depends on how successful we’re going to be and how aggressive the need for a vaccine will be. In the most optimistic scenario, we could have a licensed vaccine in one year. Reasonably in 18 months. Conservatively, I think in three years we should have a licensed vaccine.”
Rappuoli’s estimate is in line with what other experts have expressed since COVID-19 overtook the United States: late 2021 or 2022, as a best-case scenario. “It’s not going to be easy,” Hotez says. “It’s going to have to be a very carefully orchestrated dance between the epidemiological models, the scientists, the business community, and government leaders to work this out. It’s doable, but it’s not going to be easy.”
Tackling the coronavirus is also going to require far more than the development of a vaccine. Regardless of any absolutist reassurances Trump or his administration may relay to the nation, there are no black-and-white answers for how to move past COVID-19. The economy will not magically return to where it was a year ago as businesses begin to reopen, nor will society suddenly shed fears of dense gatherings when officials relax stay-at-home orders. The creation of a safe, effective vaccine, whenever it happens, will be one of many steps — albeit a crucial one — on what will inevitably be a years-long journey out of the fog of the pandemic. This is an important reality to accept for Americans desperate for a return to a normalcy.
“We have to get over this idea that everybody just hunkers down for a year and then one day the vaccine is available and everybody goes on a picnic on the National Mall,” Hotez cautions. “It’s not going to work that way.”