Dr. Ken Rosenberg became a psychiatrist because of Merle, his late older sister who suffered from schizophrenia. But did the documentarian and Cornell Weill Medical College doctor set out to tell Merle’s story in Philadelphia when he began shooting Bedlam, his new documentary on the troubled American mental-health system, nearly eight years ago?
“No, never!” Rosenberg told me during a phone interview on Monday. “Years into the project, that was not my intention.” Rosenberg had done some film work in the 1990s, but until Bedlam premiered Monday night on PBS’ Independent Lens, he hadn’t released one in 20 years. When he began the film, he looked at Los Angeles, and how life for many of its mentally ill citizens was a revolving door between emergency rooms, jails, and the street. Along the way, he took his reporting outside California, to New York and Hawaii, but it wasn’t until nearly the end that he decided to include the trauma his sister and family suffered — going back to Philadelphia, and remaking the film that he’d already edited. Together, it offers a vital and intimate perspective to a problem that, too often, the public and our politicians are content to lock away in a jail cell.
But what effect did injecting his own story into Bedlam have on Rosenberg himself?
“Oh, my God — it was so therapeutic, so liberating. I mean, what could be more therapeutic than sharing your story, but also having that story to help other people?”
Even as he sought to expose, Rosenberg also learned quite a bit. In the accompanying book to Bedlam, which he published last October, Rosenberg writes that he “failed to appreciate our criminalization of people with mental illness, which refers to putting them in jails and prisons instead of institutions of healing.”
I spoke to him at length about both the film and the book, which is currently available via PBS on-demand. Our conversation has been edited for clarity and length.
It is certainly relevant today, given the current coronavirus pandemic, that the largest mental health facilities in the country right now are our jails. How dangerous is that for the patients and society at large, especially now?
We’ve made it a crime to have mental illness. And that’s really a shame on us. There’s a lot of shame about mental illness per se. People hide it or keep it a secret. But really, we ought to be ashamed of how we treat people with serious mental illness. And it’s absurdly and unnecessarily dangerous.
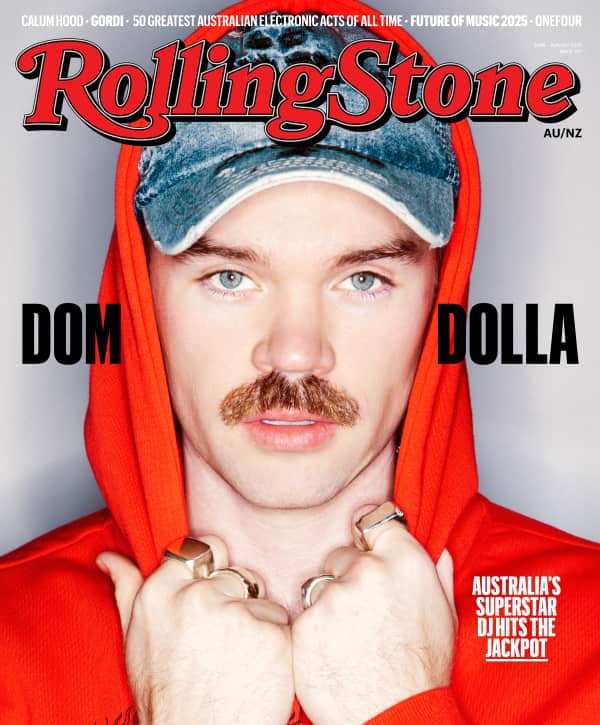
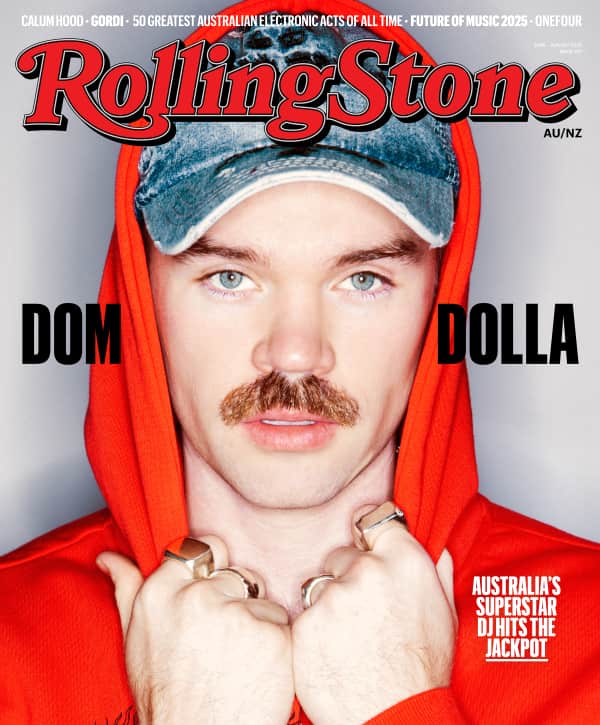
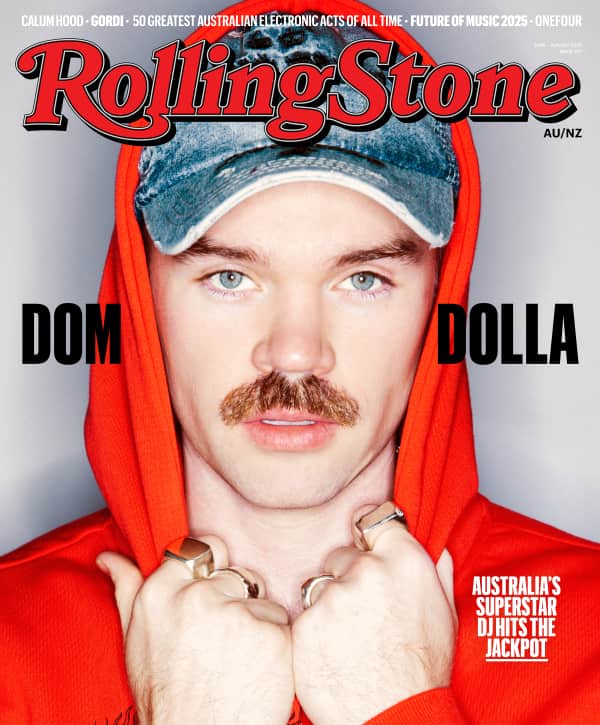
Love Music?
Get your daily dose of everything happening in Australian/New Zealand music and globally.
Right now, the three largest mental institutions in the United States are the three largest jails. The jail in Los Angeles [County] is the largest mental institution in the country. If you have a mental illness here, you’re 10 times more likely to be in jail than you are to be in a hospital. If you’re a person of color, the statistics are even greater. Twenty to 50 percent of all fatal police shootings involve someone who has a mental illness. So, our response to mental illness is really harmful. And like many other things in medical care in this country, it does a very poor job.
Now, in this time of COVID-19, it becomes very obvious that we’re all connected. That if one person has a problem in one part of the world, we all have a problem. I think the bigger issue is people with serious mental illness. How do you expect people to shelter in place when they have no shelter? [There are] 350,000 Americans with mental illness who are homeless. So, I think that the COVID-19 crisis really reveals the gaps in our system. Studies have shown over and over again, it’s very expensive to treat someone in emergency rooms and [in] jails. That’s really expensive and ineffective; it’s much cheaper to give them housing, to treat them in community mental health centers, and to treat them in hospitals.

Director Dr. Ken Rosenberg. Photo credit: Taylor Jewell/Invision/AP/Shutterstock
Taylor Jewell/Invision/AP/Shutterstock
To what degree do you feel as though our societies treat mental illness in this way because those who don’t suffer from serious mental illness are motivated by either money, a need to feel superior, or just ignorance or disrespect?
Yeah, I think that’s a great question. I think it’s a complicated question. It has to do with the fact that these are bad diseases that are not curable. So the approach that we’ve taken is to abandon these people, because whatever resources you put in, doesn’t seem to help them much. It’s not a very good approach, but I think that’s part of the issue.
And I think that you’ll see in other developed countries, they have a much more informed approach. In the book, we talk about a small community, Trieste, in Italy. It has 220,000 inhabitants, but they’re a world-health exemplar for community mental health. It actually doesn’t even need hospitals. They have a few hospital beds, but hardly have a need for them, along with putting people in jail. So there are better ways to do it.
I can’t say we’ve done it intentionally, but I think as a consequence, we’ve relegated people with mental illness to the highest bidder. As a consequence, definitely, we have said “You take care of it” to the prisons and jails, “You take care of it” to the pharmaceutical company, “You take care of it” to the police, who are the first responders for people with serious mental illness. What other medical condition is there where the first responders are law enforcement, not EMS workers?
What beyond your personal experience with your family and your sister motivated you to want to tell the story?
That’s a great question. In, like, 2010, 2011, I was on my way towards divorce. My kids were fully launched. My practice was great. I stopped making films in 2000. I made a whole bunch for HBO in the Nineties and a couple for PBS before that, and stopped doing it just to kind of focus on my practice and, you know, live in the suburbs. But then when I was getting divorced, I decided, “I should do something, use my skills as a filmmaker and as a writer — and what would be the most important story I could tell?” The answer was very simple. I should tell a story about people with serious mental illness like my sister, who we have abandoned and neglected our society.
To me, it seemed like the civil-rights movement that ought to be happening that isn’t. That has been the struggle for people with serious mental illness; the discrimination against them, both in terms of how we treat them as disabled people, but also how we fail them completely from a medical standpoint. To me, it’s just mind-boggling, where, you know, because we have the sickest people, [who] the psychiatrists don’t treat [in their private practices]. Nowhere in medicine does that happen. You know, when you say, “Oh, we’re gonna just treat people with mild chest pain, but forget the people who need, you know, bypass surgery.”
Can you tell me what you learned in the process of both shooting the film and, later, writing the book?
You know, this may sound really trite, but I found that goodness triumphs often, especially when it’s combined with perseverance. Whenever I film someone [with mental illness] I say, “Let me speak to your family, let me ask them if it’s OK.” I understand, perhaps more than most people, that mental illness — particularly serious mental illness — is a family disease that involves everyone in the family.
I also learned more about the criminalization of people with serious mental illness. I don’t think I fully realized until I lived it, until I saw it, how we’ve made serious mental illness a crime. Patrisse [Cullors, the Los Angeles activist and co-founder of Black Lives Matter who is featured in the film] was really remarkable. [When we interviewed her], she hadn’t become what she was going to become, which is one of the most prominent mental health and decarceration activists in the world.
Were there things that weren’t included in the film? Things that, perhaps, were too difficult to show?
The last one I did for HBO was a film on psychotherapy [2000’s Drinking Apart: Families Under the Influence]. And that was for families. It’s very, very hard to show psychotherapy. It’s like a slow sailboat race. There’s not much drama in it. It’s very hard to capture, and I would like to have captured that [in Bedlam]. Also, peer support is a really good thing. I would have loved to have seen patients themselves go off and help other patients in peer-to-peer support.
But the discipline that one has to take as a filmmaker, as a writer, you have to kind of let the story tell itself. You can’t really push everything into it. I’m so grateful that we end the film on the optimistic note of advocacy. That’s what’s going to make a change. I could not have scripted Patrisse to stop a $3.5 billion jail. And I could not have predicted that the [doctors] in the emergency room would be the same people at the end of the film pleading with [Los Angeles County] to focus on mental health.
Early in the film, it’s pointed out how President Richard Nixon didn’t take mental illness seriously, and essentially left it to the states.
You’re being generous — he had no idea about mental illness. Nixon had absolutely no friggin’ idea about it.
How do you bridge that ideological divide?
Well, I think the simple answer is that you can’t, but I will say that I think that it wasn’t just Nixon — for a lot of people, the problem was that they really weren’t continually dedicated to people with serious mental illness. I don’t know if it’s a Republican or Democratic party issue. I think it’s just a stupidity issue.
Let’s say you don’t even give a darn about human life. Let’s say you just want to save money. Then you don’t leave people on the streets and in the emergency rooms and in the jails and the prisons. And if you want to save lives, of course, that’s not what you do. It’s just plain ignorance. Honestly, I think there’s people who are not thinking clearly about it. They’re thinking, maybe, about the next election.
What has to change is not in the government. It’s in us, the citizens. We need to become advocates for people with mental illness. And we see that in cancer. You know, it wasn’t Nixon’s war on cancer that made breast cancer a much more treatable and manageable disease. It was the relentless advocacy of people with cancer. Same thing happened with HIV. It wasn’t the death of Roy Cohn that made HIV a much more manageable, although [still] a difficult, disease than it was 20 years ago. Right. It was relentless advocacy, relentless activism. And that’s really what we need.
To that point, I want to ask you about the stigma of mental health in this country. It is easy to see how one might almost be tempted to laugh when you see some of the behavior by patients in the film. And there’s obviously a lot of media speculation and interviews with people in your field about the mental state of the president. What do you think about that?
I think, thank God, we live in a democracy and if someone has an illness, especially as the president — maybe something that has to do with narcissism, for instance — I think it’s a reasonable thing to talk about. On the other hand, I think to hurl diagnosis as insults really hurts what we’re trying to do here.
We’re trying to say that these are illnesses. These are not character flaws or insults. Their disease needs to be compassionately understood and treated.
How do we break out of that mode of thinking and speaking, collectively?
I think that’s something we need to unlearn as kids and adults. And I think that’s increasingly the case. I mean, I think that’s because mental illnesses are less stigmatized now than they used to be. We’re more open-minded about the kids who have psychiatric illnesses — whether it’s ADHD or bipolar disorder, or whatever it is. Depression. We’re more talking about it. And that creates the space for early intervention, as opposed to, you know, you have to hide that. But if we believe these are medical illnesses, you don’t call someone “an f-ing diabetic,” right? We’d say, “What are you saying? That doesn’t make any sense.” Somehow, we’ve made it OK to discriminate and have slurs against people with mental illness.