Anxiety is soaring across the country as the number of confirmed cases of the new coronavirus continues to climb. City, state, and federal governments are scrambling to contain the virus, also known as COVID-19. The government’s response to the coronavirus pandemic has lagged behind that of other affected countries, raising questions about why there have been delays in testing and how long it will take to slow the virus’s spread.
For people who are at risk of developing serious complications from COVID-19, such as older people and people with underlying health conditions like heart disease or diabetes, the guidance from the Centers for Disease Control and Prevention (CDC) is clear: avoid large crowds and non-essential travel, and stay indoors as much as possible. But it’s less clear how people who do not fit into those categories should operate on a day-to-day basis. For now, the biggest question many people have is: How should I go about my life? Am I at risk? Should I go to my friend’s birthday party this weekend? Should I take my young child out to the park? If I’m a healthy person in my twenties, thirties, or forties, why should I change my lifestyle?
Rolling Stone interviewed medical doctors, public-health experts, and researchers to help answer questions about daily life during the coronavirus pandemic. These experts caution that there are no cure-alls or one-size-fits-all solutions. They also say that as more tests are completed and more data becomes available, we will likely learn more about the virus, the ways it can be transmitted, and its effect on healthy and sick people.
But we know enough about the virus to help answer questions the average healthy person might have.
How cautious should I really be about getting COVID-19?
It’s time to embrace your inner germaphobe. The most important thing right now, public-health experts say, is slowing the transmission of the virus and protecting those who are vulnerable — namely, people over the age of 70, people with pre-existing conditions, and people with weakened immune systems.
What does that mean in practice?
Wash your hands for 20 to 30 seconds, with soap, ideally every hour. Don’t touch your face. Keep a six-foot distance from other people out in public. Disinfect your phone and your shopping cart at the grocery store.
Donna Petersen, the dean of the University of South Florida’s College of Public Health, says if you can work from home, you probably should. If you can avoid large gatherings, you probably should. When you need to run errands like grocery shopping, try going during off-peak hours if you can. You don’t have to go full J.D. Salinger and become a recluse. But minimize risk as much as you can, including by avoiding interpersonal encounters that aren’t essential.
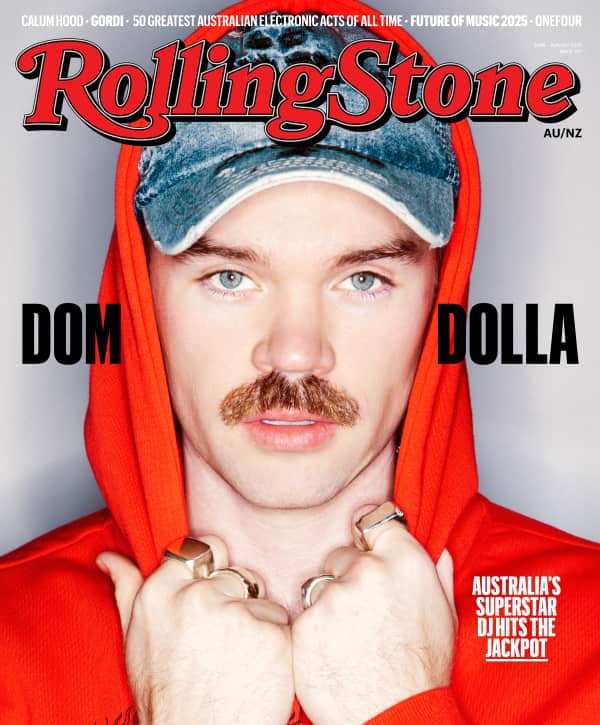
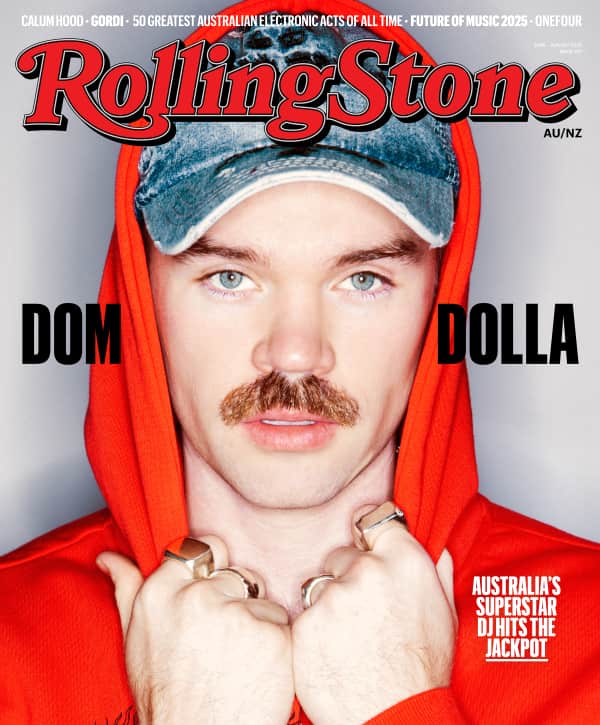
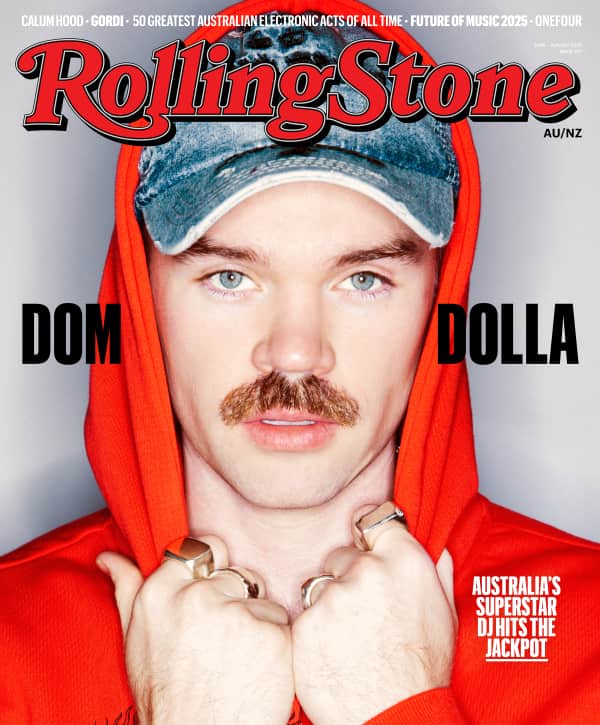
Love Music?
Get your daily dose of everything happening in Australian/New Zealand music and globally.
“Do you need to lock yourself in?” Petersen says. “No. Not based on what we know today. But people need to think: Do I really need to do this? If you play out the worst-case scenario, will you say it was worth it to have done that?”
For a healthy person in their twenties, thirties, or forties, how bad would it be if they got COVID-19? How does it compare to the regular flu or another common illness?
COVID-19 is a completely different virus and belongs to a different family of viruses even though it’s still a respiratory pathogen, says Dr. Seema Yasmin, an assistant clinical professor of medicine at Stanford and a former investigator for the CDC’s Epidemic Intelligence Service. Regular flu is really bad for the very young and very old, but COVID-19 appears to be sparing young children.
Based on the current data, 95 percent of people who get the coronavirus will experience mild to moderate symptoms, says Sandro Galea, the dean of Boston University’s School of Public Health. Some people will get the coronavirus and not even know they have it.
A bad case of coronavirus for a healthy person will likely be no worse than a bad case of regular flu, Galea says, causing a headache, fever, soreness, nausea, and a cough. You will recover from it in a matter of days (again, based on the current data).
Unlike the regular flu, there is no vaccine for COVID-19, says Dr. Sarah Fortune, the chair of the Department of Immunology and Infectious Diseases at Harvard’s T.H. Chan School of Public Health. “Many people are working on a vaccine,” she says. “But developing a real vaccine that we know is safe and we can make enough of it to go into lots of people is a complicated undertaking, and that is at least a year, probably longer, at least a year away.
Right now, Fortune says, there is a bit of a misconception about what the coronavirus means for the vast majority of the public. The reality is: Most young people — and almost all children — can be infected with this virus and be fine, Dr. Fortune says.
“People think of this as the contagion: I’m going to get it and drop dead,” she says. “For the vast majority of people, that’s just not true.”
Here’s the caveat: Fortune, Galea, and other experts say that as more tests are conducted and more data comes in, our understanding of the coronavirus could evolve. But for now, they say the virus’s direct effects on healthy people aren’t a big concern.
Why should I change my lifestyle if I’m not at serious risk from the virus?
Even if you’re not at risk of major health outcomes or death, healthy people play an absolutely critical role in protecting those who are especially vulnerable to the coronavirus.
Dr. Fortune of Harvard uses the example of colleges and universities. Why should they close if many of the people on those campuses are young adults who are at low risk of being seriously affected by coronavirus? It’s all about stopping the transmission of the virus, Dr. Fortune says.
“The problem is that those [college students] can become amplifiers of viral transmission in the community,” she says. “There are obviously people in the community” — older faculty, food-service workers, facilities employees, bus drivers — “who are much more vulnerable and who will not be fine because they’re old or immunocompromised or just unlucky.”
Public-health messages are often framed in terms of personal risk: work from home because you are at risk, wash your hands because you are at risk. But the key message with coronavirus is that we all need to take extraordinary measures to slow the spread and protect the larger community.
“We should be thinking to ourselves a little bit like the World War II mentality: One for all, all for one,” she adds. “This is a community effort, not an individual protection reflex.”
Which should I rely on for information to get through the pandemic, the Centers for Disease Control or the World Health Organization?
Public-health experts say that even though the CDC has faced criticism for its sluggish response to the coronavirus, CDC’s website is still the gold standard when it comes to reliable and up-to-date information during a pandemic.
Donna Petersen, the University of South Florida public-health expert, says both organizations offer helpful and actionable data, and both can be trusted. She notes that the CDC, as the flagship health organization for the U.S., will offer more detailed information tailored to an American audience while the WHO provides information to a range of nations across the world.
Sandro Galea, the dean of Boston University’s School of Public Health, says he encourages everybody to pay specific attention to what the CDC publishes on its website.
In short: More CDC and less Twitter.
You can access the CDC’s coronavirus-specific website here.
You can access the WHO’s coronavirus-specific website here.
Should I go to my friend’s birthday party at a bar tomorrow?
What kind of bar are you talking about? A barely occupied, dust-ridden Irish pub with cheap Jameson on the rocks? Or a trendy gastropub that is so crowded you have to wait 40 minutes to get a pricey Moscow mule?
Current CDC guidelines recommend that people remain between six to 10 feet away from each other at all times; if you can do that while getting your drink on, that’s a lot more preferable than standing shoulder-to-shoulder in a crowded bar. That said, at a party where you’re having frequent (albeit more likely than not, boring) conversations with other guests, it’s gonna be pretty difficult to do that within a six-to-10-foot radius, so the answer is, it’s probably not a good idea to go to parties right now.
Generally speaking, the concept of social distancing — the tactic that was effective at reducing the spread of the virus in places like China and South Korea — is dependent on citizens reducing their social contact and spending as much time as possible at home. The goal is to prevent a huge increase in new infections so as not to overwhelm the health care system, something epidemiologists refer to as “flattening the curve.”
Currently, “the likelihood of widespread community transmission remains very low,” says James Scott, an associate professor at the Dalla Lalla School of Public Health. “But this is likely to change over the next month.” To do your part in flattening the curve, it’s smart — not to mention socially responsible — for you to avoid as much social contact as you can in the coming weeks, including, yes, your Thursday happy-hour habit.
Can I still go to the gym? What if I disinfect all the surfaces I use and stay away from other people and wash my hands before I touch my face?
Again, as is the case with any public place, it all depends on risk reduction. The 6 to 10 feet away rule still applies here, and while that’s a little bit easier to do at a gym than it is at, say, a bar or a concert, it’s better to go during off-hours, such as early in the morning or later in the evening, rather than at a time when it’ll be packed to the gills with hard-bodied millennials eager to get a few miles in. Disinfecting before and after you use machines is also key. (Most gyms are pretty orthodox in their approach toward hygiene as is, but you can never be too sure).
That said, in keeping with the theme of social distancing, the key to slowing down the spread of COVID-19 is to reduce contact with other people as much as possible so if there is a way for you to work out without having to go to the gym, now is the time to pursue it. Biking, running, and jogging on a nearby track or park are all great options. You can also find tons of great subscription services for streaming workout classes like the Daily Burn, or, if you’re really cheap, just cop a bunch of yoga videos off YouTube.
Do we stop sending our kid to preschool? I’m a stay-at-home parent and I can stay home with our kids and keep them completely away from the public, but should I?
This is a question that is being debated by public health experts and state and city officials across the country right now, probably literally as we speak.
It’s true that COVID-19 thankfully appears to pose far less of a risk to children, producing only mild symptoms in those who have contracted it. In fact, according to Chinese data, while children constituted about 2.5% of the country’s COVID-19 cases, only 0.2% of children became critically ill, a blessedly minuscule number.
This is in part why officials in cities like New York have been reluctant to shut down public schools, with many schools either choosing to shut down as a precautionary measure (similar to many colleges and universities) or shutting down only following cases of confirmed exposure or spread. There are some who believe this is unwise, like Yale University sociologist and physician Nicholas Christakis, who told NPR that “if you wait for the case to occur [in your school], you still have wound up closing the school, but now you’ve missed the opportunity to have the real benefit that would have accrued had you closed the school earlier. It’s sort of closing the barn door after the cow is gone.”
But many school district officials argue that the benefits of keeping schools open as long as possible outweigh the risks, particularly for low-income children who may rely on school meals for breakfast, lunch, and in some cases dinner. School closure also places a tremendous burden on working parents, many of whom aren’t able to work remotely and will have to go in to their jobs as usual, requiring them to pay for child care.
Bottom line: This is a complicated issue that is still being negotiated as we speak, and whether or not you want to pull your kids out of school for the time being is dependent on lots of different factors, such as whether you have the financial means necessary for child care. But in the event that schools do close across the country or in areas with lots of COVID-19 clusters, it’s still OK to take them to public spaces like parks, says Scott (museums, which are increasingly being subject to closure, are a different matter). “Outdoor activities are relatively lower risk than indoor activities where multiple people may be present,” he says. “It is still very safe to go outside for a walk as long as you steer clear of crowds.”
Why has it taken so long to get test kits into the hands of medical professionals?
There are a number of issues at play here, says Dr. Karen Kaul, chair of the Department of Pathology and Laboratory Medicine at North Shore University Health System in Illinois and a spokesperson for the College of American Pathology. One of those issues is just how quickly the COVID-19 situation is evolving: “Part of the challenge is the fluid situation and the dramatically rising number of patients we’re seeing in this country,” she says. This is a brand-new virus, so labs must come up with brand-new testing protocols, and it takes time to ensure their reliability and accuracy.
Another part of the issue is that there isn’t one centralized system being used to generate test kits right now. Currently, there are a few ways to be tested for COVID-19: you can have testing sent to a public health lab using a CDC kit; or you can have it done in a hospital lab using a lab-developed test. You can also use a kit manufactured by a diagnostics company and approved by the FDA for emergency use, but as of the time of this writing these tests are not yet available, though that will hopefully change soon, says Kaul.
In states like Illinois, there are more coordinated efforts to have hospitals and public health labs working closely together. Right now, there is only a limited amount of public-health test kits available, and the rollout has been shaky at best: The FDA commissioner has said that the CDC has shipped 75,000 tests to public health labs — far fewer than the million-plus promised by the Trump administration, and some of which were only given to high-risk patients or delivered inconclusive results.
Hospital lab-developed tests also must adhere to a strict set of guidelines such as those put forth by the College of American Pathology to validate the tests, meaning they need to test positives and negatives and assess their sensitivity and specificity (the positive identification versus negative identification rates) to make sure they are accurate. This is crucial to the testing process, and though about 20 labs so far have gone live with such testing, “there is a fair bit of work that needs to be done” before many laboratories can do this, says Kaul. The tests for COVID-19 are also more complicated than the typical testing hospital labs are able to do. “It’s looking at viral RNA and using PCR and so forth so it’s not your typical hospital laboratory test,” she says.
Luckily, says Kaul, the FDA has streamlined the process for testing approval: “in the past it’s usually something that takes months and I think we’re hoping it’ll be a matter of days for hospital labs,” she says. Recently, the Cleveland Clinic also announced it had developed a test that would produce results in a matter of hours rather than days, as was previously the case for other tests.
Still, Kaul says there remains a “deficit” of available tests for the public. “We need to be cautious about the messaging here because many labs are working on tests, but many tests are not yet available,” she says.
I’ve seen a lot of coverage on how to not go stir-crazy working from home and not to touch my face, but I still have no idea what I should do if I start showing symptoms other than self-quarantine. What is the procedure for seeking help and getting tested?
Because of the dearth of available testing kits, medical professionals are primarily “focusing on testing people who are symptomatic,” i.e. people with a dry cough, fever, and/or chest pain/tightness, says Kaul.
What this essentially means is that if you have a friend of a friend of a friend who may have tested positive for COVID-19 and you want to alleviate your stress about the whole situation but you’re feeling pretty much fine, sorry, but there’s no reason at this time for a physician to give you a test. Same goes if you just have mild cold/flu symptoms, such as a runny nose or a slightly scratchy throat — yes, you absolutely want to stay home, but no, you don’t need to go running to your ER to get a COVID-19 test.
If you do have distinct COVID-19 symptoms, you should call your physician, who will ask detailed questions about your symptoms and potential exposures. Experts stress the importance of calling first, which can help prevent putting too much strain on the health-care system, says Donna Petersen of the University of South Florida.
“Anyone that has symptoms should call — call — a health provider first,” Petersen says. “They will ask you questions, and guide you on next steps for what you should do.”
Unfortunately, due to the limited number of available tests and current federal guidelines for when testing is appropriate, whether or not you’ll actually be tested is dependent on numerous factors, including the individual doctors/hospitals and if you meet various criteria. Currently, the CDC defines a “patient of interest” as someone who is symptomatic and has known exposure or a history of travel to affected areas, but “as things evolve and it’s changing day to day, I expect we’ll see those criteria broadening as we are more cognizant of what’s going on in the community with spread,” Dr. Karen Kaul says.
Can you get it from water?
Over the past few days, many people have stocked up on bottled water, but this is probably not for any good reason other than sheer panic-buying. Your water is likely not going to get turned off even in the worst case scenario, and unless you live in a home where water isn’t readily available, it isn’t necessary to buy cases upon cases of bottled water. Instead, focus on stocking up on non-perishable household goods in the event of a quarantine. (Check out these guidelines for inspiration.)
“Water distribution systems are likely to remain very safe,” says Scott. “There typically are not points in these systems where contaminants can enter, and there is (or should be) chlorine residual that would provide protection even if something minor did get in.”
There is, however, one caveat: the water from your toilet, as there is evidence the virus can be transmitted via fecal matter, says Scott. “The general population does not normally have contact with wastewater except at the ‘point of production’ (e.g., ‘toilet spray’ — so put the lid down before you flush if you have the virus!),” he says. “Bleach is highly effective.”
Should we be sanitizing debit cards/credit cards?
COVID-19 can remain viable on surfaces for hours or days, according to the CDC, which is why some people have suggested it may be a good time to engage in cashless transactions.
But can it live on your credit card? Good question, says Scott, but “the buttons on the bank machine and credit card terminals probably present a much greater risk of transmission” than your bank card or credit card, which is usually only used by you or maybe one or two other parties. “Wash your hands after you use these devices or wear gloves if you’re really concerned.”
Should I cancel my meals-by-mail service (Blue Apron, HelloFresh, etc.) or stop ordering food for delivery? Can it survive in food?
It’s not clear at this time that COVID-2019 can be transmitted via food. In late February, the FDA reported they were not aware of coronavirus transmission via food or food packaging. That said, it’s certainly not outside the realm of possibility that an infected person could transmit it if they didn’t wash their hands before preparing a meal.
In the case of hot food, the virus would likely be killed by cooking, while delivery services preparing fresh ingredients, such as HelloFresh, are being vigilant. “We have implemented additional safety measures such as more frequent handwashing and sanitation of our facilities, along with limited access to our production site,” a spokesperson tells Rolling Stone. Blue Apron assures customers that they are adhering to all FDA guidelines. “We continue to closely monitor guidance provided by the FDA and the Centers for Disease Control and Prevention and other applicable government agencies,” they wrote.